Highlight
1. This large nationwide cohort study analyzed 8612 patients treated with PD-L1 inhibitors atezolizumab or durvalumab combined with chemotherapy for extensive-stage small cell lung cancer (esSCLC) in France.
2. No clinically meaningful differences were observed in effectiveness outcomes such as time to treatment discontinuation and overall survival between atezolizumab and durvalumab.
3. Safety profiles, including immune-mediated side effects requiring systemic steroids and all-cause overnight hospitalizations, were comparable between both treatments.
4. Findings suggest that treatment choice between atezolizumab and durvalumab can consider local availability, institutional protocols, and cost without impacting clinical outcomes significantly.
Study Background
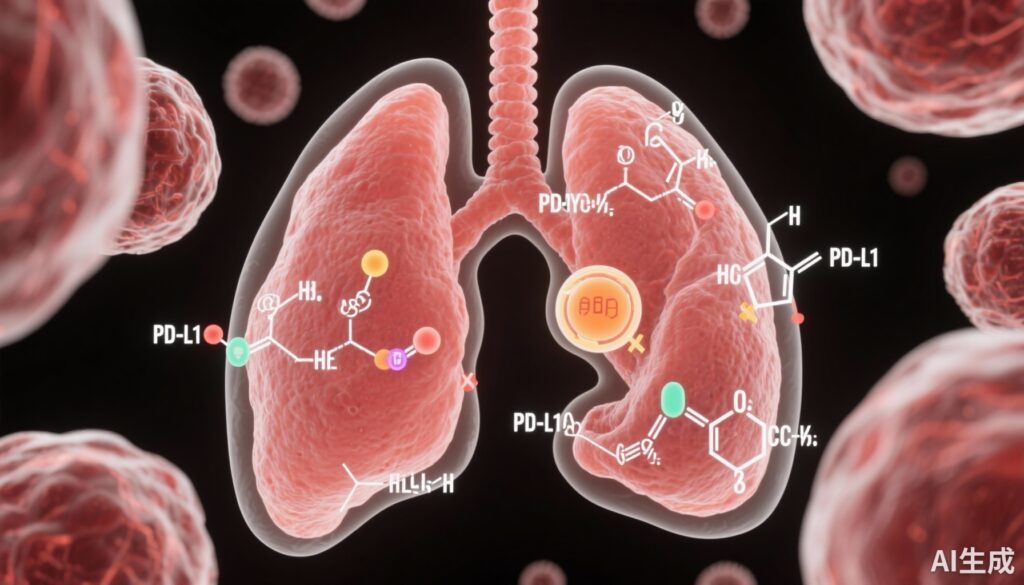
Extensive-stage small cell lung cancer (esSCLC) is a highly aggressive malignancy characterized by rapid progression and poor prognosis. Despite initial sensitivity to chemotherapy, development of resistance leads to high relapse rates and mortality. Historically, cytotoxic chemotherapy was the standard first-line treatment but achieved limited survival benefits. Recently, integration of immunotherapy targeting the programmed death-ligand 1 (PD-L1) pathway, particularly with atezolizumab and durvalumab combined with chemotherapy, has marked a paradigm shift for esSCLC management based on pivotal randomized controlled trials demonstrating improved overall survival.
However, direct comparative effectiveness and safety data on these PD-L1 inhibitors in real-world practice are lacking. Variations in patient characteristics, comorbidities, and treatment administration outside clinical trial settings can influence outcomes substantially. Comprehensive nationwide observational studies are crucial to validate efficacy and assess safety profiles in broader populations, thereby informing clinical decision-making.
Study Design
This retrospective cohort study utilized the French National Health Data System (SNDS), encompassing all patients with esSCLC who initiated first-line treatment with atezolizumab or durvalumab combined with chemotherapy between May 1, 2019 and December 31, 2023, with follow-up through June 30, 2024.
Baseline demographics, including age, sex, and clinical characteristics, were documented. The primary effectiveness endpoints were time to treatment discontinuation (TTD) and overall survival (OS). Safety was evaluated via rates of all-cause and cause-specific overnight hospitalizations, including those related to immune-mediated adverse events, inferred from systemic steroid use.
The study included 8612 patients: 5188 received atezolizumab and 3424 received durvalumab. Median follow-up times aligned with clinical practice standards, enabling robust survival analyses. Cox proportional hazards models adjusted for potential confounders were employed to compare outcomes between the two PD-L1 inhibitors.
Key Findings
Patient Population: The mean age was 66.2 years (SD 8.7) and majority were male (63.8%). The large patient number and nationwide scope ensure representative data reflecting routine clinical use in France.
Effectiveness: Median time to treatment discontinuation was similar: 5.4 months (95% CI, 5.3-5.5) for atezolizumab versus 5.5 months (95% CI, 5.4-5.6) for durvalumab. The adjusted hazard ratio (aHR) for treatment discontinuation comparing durvalumab to atezolizumab was 0.97 (95% CI, 0.92-1.02), indicating no statistically significant difference.
Median overall survival also showed no meaningful difference: 11.1 months (95% CI, 10.6-11.4) for atezolizumab versus 11.4 months (95% CI, 10.9-11.9) for durvalumab, with an aHR of 0.93 (95% CI, 0.88-0.98) favoring durvalumab but of limited clinical significance given overlapping confidence intervals.
Safety: A high proportion of patients (61.8%) received systemic steroids during treatment, reflecting immune-related adverse event management, with similar frequency between groups. No statistically significant differences were observed in rates of all-cause or specific cause overnight hospitalizations, underscoring comparable toxicity profiles. These real-world safety data align with existing clinical trial evidence and support predictable tolerability of both agents.
Expert Commentary
This large-scale, real-world cohort study provides compelling evidence that atezolizumab and durvalumab combined with chemotherapy offer comparable clinical benefit and safety in the first-line treatment of esSCLC. While modest differences in hazard ratios were noted, their magnitude does not translate into meaningful clinical distinctions, supporting therapeutic interchangeability.
These findings are important given the paucity of direct head-to-head trials comparing these agents. The use of nationwide administrative health data lends strength in terms of generalizability and captures routine clinical practice, including heterogeneous patient populations traditionally underrepresented in clinical trials.
Caveats include the observational design which may be subject to residual confounding despite statistical adjustments. Additionally, detailed data on tumor PD-L1 expression, performance status, and genetic biomarkers were unavailable, potentially limiting nuanced subgroup analyses.
Current guidelines endorse both atezolizumab and durvalumab as standard of care for esSCLC, and this study reinforces their equivalence. Clinical decisions may therefore justifiably consider logistical aspects such as drug access, institutional protocols, administration convenience, or economic factors without compromising patient outcomes.
Conclusion
This nationwide French cohort study demonstrates no clinically relevant differences in effectiveness or safety between atezolizumab and durvalumab when combined with chemotherapy for first-line treatment of extensive-stage small cell lung cancer. Both PD-L1 inhibitors can be viewed as interchangeable therapeutic options in routine practice, enabling flexible treatment selection informed by healthcare system factors rather than efficacy or toxicity concerns alone.
Future research could focus on identifying biomarkers to personalize PD-L1 inhibitor choice and investigating combination strategies to further improve survival outcomes in this challenging malignancy.
Funding and ClinicalTrials.gov
This study was conducted without external funding. The research utilized existing national health data resources and thus was not registered as an interventional clinical trial.
References
Jourdain H, Albin N, Monard A, Desplas D, Zureik M, Haddy N. PD-L1 inhibitors combined with chemotherapy for extensive-stage small cell lung cancer: a French nationwide cohort study. Lancet Reg Health Eur. 2025 Oct 9;59:101484. doi:10.1016/j.lanepe.2025.101484. PMID: 41142658; PMCID: PMC12547005.