Introduction
Metastatic hormone-sensitive prostate cancer (mHSPC) represents a critical stage in prostate cancer requiring intensified systemic therapy. The advent and expanded approval of androgen receptor axis-targeted (ARAT) agents—such as darolutamide, abiraterone, apalutamide, and enzalutamide—have meaningfully advanced treatment options beyond traditional androgen deprivation therapy (ADT). Additionally, chemotherapy with docetaxel has been incorporated into regimens to improve outcomes. Yet, an important clinical question remains: Do older patients with mHSPC, often facing increased comorbidities and frailty, derive comparable benefit from these intensified doublet or triplet therapies as younger counterparts?
Study Background
Prostate cancer incidence is higher among older men, who often present with metastatic hormone-sensitive disease. Treatment intensification with combined modalities aims to improve overall survival (OS); however, older patients may be more susceptible to adverse events and schedule disruptions due to toxicity. While randomized controlled trials (RCTs) have demonstrated benefits of doublet therapies (ADT plus ARAT or docetaxel) and emerging triplet therapies (ADT plus ARAT plus docetaxel) in the general population, evidence focusing specifically on older patients (≥70 or 75 years) has been limited.
Study Design
Zhou et al. conducted a systematic review and network meta-analysis incorporating 11 RCTs evaluating combinations of ADT with ARAT agents and/or docetaxel in older patients with mHSPC. Eligibility criteria required age thresholds (≥70 or 75 years), with overall survival as the primary endpoint. By pooling data across trials and employing a random-effects model, indirect comparisons between therapeutic regimens were estimated. The analysis focused on OS hazard ratios (HRs) and rankings via P scores to identify the most effective treatments in this population.
Key Findings
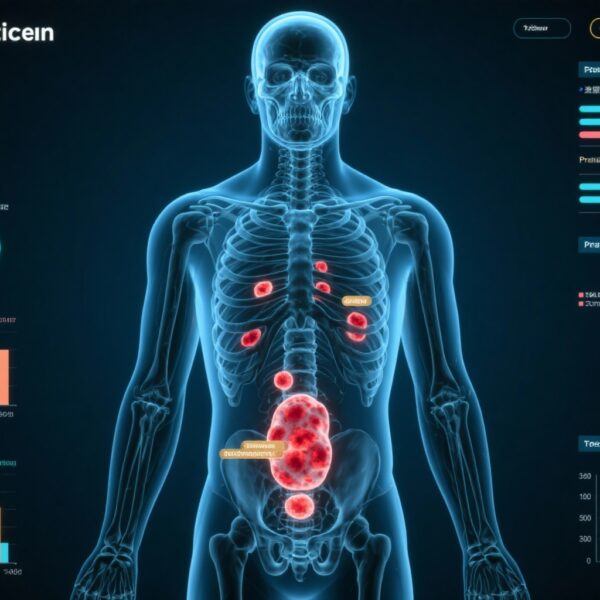
The analysis yielded several pivotal insights:
1. Darolutamide-based triplet therapy (darolutamide + ADT + docetaxel) demonstrated a significant OS benefit compared to both ADT alone (HR 0.47; 95% CI: 0.28-0.77) and ADT plus docetaxel doublet therapy (HR 0.61; 95% CI: 0.40-0.93). This triplet regimen ranked highest with a P score of 0.90, indicating superior efficacy among tested options.
2. Another triplet combination, abiraterone + ADT + docetaxel, showed a trend toward improved OS but did not reach statistical significance versus ADT alone (HR 0.61; 95% CI: 0.37-1.02) or ADT plus docetaxel (HR 0.80; 95% CI: 0.52-1.24). This combination ranked second with a P score of 0.67.
3. Among doublet therapies, darolutamide + ADT (P score 0.61), apalutamide + ADT (0.60), and enzalutamide + ADT (0.56) ranked higher than ADT + docetaxel (0.40) and abiraterone + ADT (0.20), which performed variably.
4. The data suggest an additive benefit of incorporating docetaxel into both doublet and triplet regimens for older men, underscoring that chemotherapy remains relevant despite the advent of novel ARAT agents.
5. Although efficacy signals favor triplet therapy with darolutamide, the study underscores the critical need to clarify toxicity profiles in older populations, given their potentially increased vulnerability to treatment-related adverse events.
Expert Commentary
This analysis provides important direction for clinicians treating older patients with mHSPC. Darolutamide’s favorable safety profile relative to some other ARAT agents—owing to its minimal blood-brain barrier penetration and limited CYP450 interactions—may partly explain its superior ranking in triplet therapy settings. The statistically significant OS benefit observed supports its integration alongside docetaxel and ADT in older patients who have adequate performance status.
However, the lack of conclusive OS benefit for the abiraterone-based triplet highlights heterogeneity in outcomes dependent on agent selection, patient characteristics, and trial designs. Risks such as hepatic toxicity, hypertension, and steroid-related side effects associated with abiraterone warrant cautious use among older adults.
Limitations include indirect comparisons inherent to network meta-analysis and the variability in age cutoffs and comorbidity assessments across trials. Furthermore, data on quality of life and treatment tolerability specific to older patients were scarce, emphasizing the need for dedicated studies on geriatric oncology endpoints.
Conclusion
For older patients with metastatic hormone-sensitive prostate cancer, triplet therapy comprising darolutamide, ADT, and docetaxel currently represents the most promising approach to prolong overall survival. While this regimen ranks highest in efficacy, clinicians must balance oncologic benefits against potential toxicity risks, mandating individualized assessments of fitness and close monitoring. Future research should focus on prospective evaluation of safety, tolerability, and patient-reported outcomes in the elderly to optimize therapeutic strategies further. Until such data are available, the inclusion of darolutamide-based triplet therapy offers an evidence-based avenue to improve survival in this vulnerable population.
References
Zhou S, Alerasool P, Kishi N, Tsao CK. Do Older Patients With Metastatic Hormone-Sensitive Prostate Cancer Benefit From Triplet or Doublet Therapy? A Network Meta-Analysis. Clin Genitourin Cancer. 2025 Aug;23(4):102380. doi: 10.1016/j.clgc.2025.102380. Epub 2025 May 30. PMID: 40545421.
James ND, et al. Abiraterone for Prostate Cancer Not Previously Treated with Hormone Therapy. N Engl J Med. 2017.
Fizazi K, et al. Darolutamide plus Docetaxel and Androgen Deprivation Therapy in Metastatic Hormone-Sensitive Prostate Cancer: ARASENS Trial. N Engl J Med. 2022.
Scher HI, et al. Apalutamide and Enzalutamide in mHSPC: Clinical Trial Updates and Considerations. J Clin Oncol. 2023.