Study Background and Disease Burden
Heart failure (HF) remains a prevalent chronic condition worldwide, characterized by the heart’s inability to pump blood efficiently. Malnutrition is a frequent comorbidity among HF patients, contributing to worsened functional capacity, increased hospitalization rates, and poor overall prognosis. The interplay between cardiac dysfunction and nutritional status is complex, involving inflammatory pathways, catabolic states, and reduced appetite. Recognizing and addressing malnutrition could potentially improve clinical outcomes and quality of life in this vulnerable population. However, robust evidence evaluating structured nutritional interventions in chronic HF, particularly those at risk of malnutrition, is limited.
Study Design
This article presents a prespecified subanalysis of the PACMAN-HF trial — a randomized controlled trial assessing the Prognostic And Clinical iMpAct of a Nutritional intervention in patients with chronic HF. Ambulatory chronic HF patients at risk of malnutrition were identified using the Mini Nutritional Assessment (MNA) questionnaire, a validated tool widely used to screen for malnutrition risk.
Eligible participants were randomized 1:1 into either an individualized nutritional intervention group or a standard care control group. The intervention consisted of tailored nutritional support designed to address the specific deficits and needs of each patient, encompassing dietary counseling and supplementation when appropriate. The control group received routine HF management without specific nutritional support.
Key clinical endpoints included a composite measure of all-cause mortality or time to first HF hospitalization, with additional assessments of nutritional status and functional capacity evaluated at 3- and 12-month follow-ups. Functional capacity was measured using the 6-minute walk test (6MWT), a validated metric reflecting exercise tolerance and prognostic outlook.
Key Findings
Out of 225 screened patients, 72 (32%) were identified as at malnutrition risk; 64 (28.4%) met inclusion criteria and were randomized (31 intervention; 33 control). Baseline patient characteristics were well matched except for a higher prevalence of hypertension in the control group (79.3% vs. 51.6%, p=0.027). The cohort predominantly consisted of patients with ischemic HF (46.9%) and moderately reduced left ventricular ejection fraction (mean 31.9%).
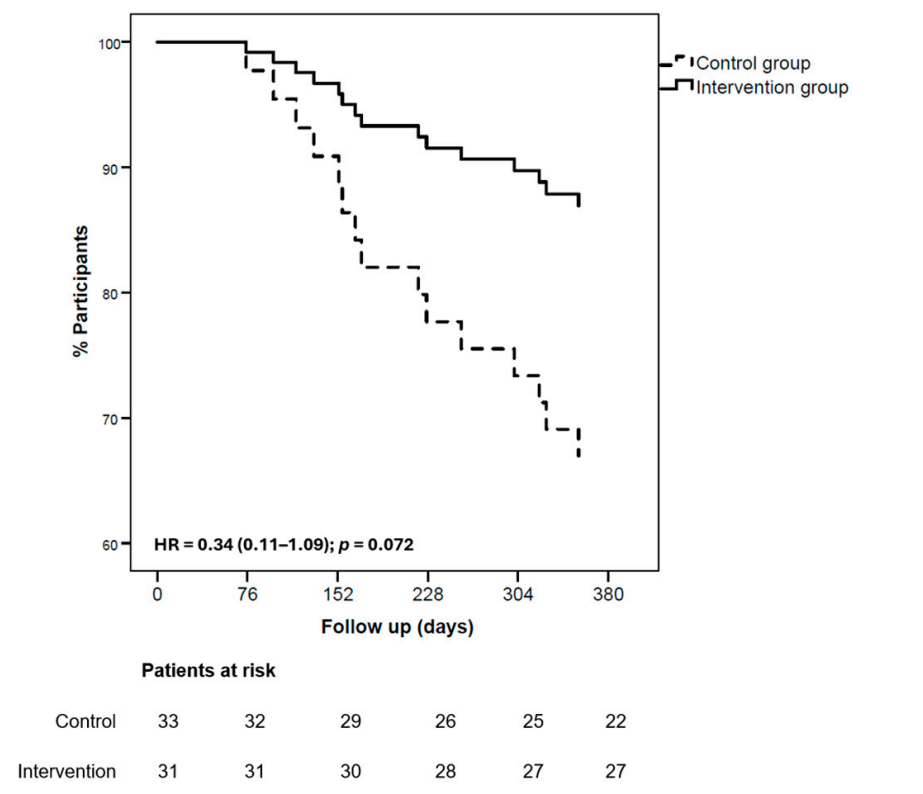
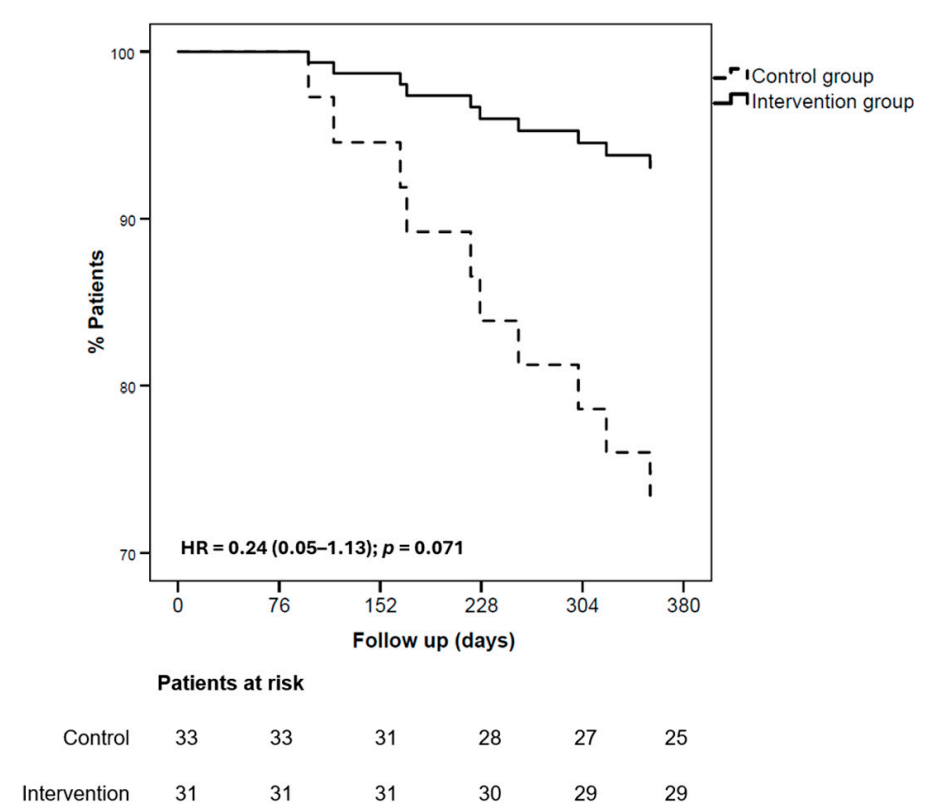
Regarding the primary composite endpoint (all-cause mortality or first HF hospitalization), there was no statistically significant difference between groups at 365 days (Hazard Ratio [HR] 0.34, 95% confidence interval [CI] 0.11–1.09; p=0.072). The endpoint occurred in 4 patients (12.9%) in the intervention group versus 11 (33.3%) in controls. The trend toward benefit was largely attributed to fewer HF hospitalizations in the intervention group (2 patients, 6.4%) compared to controls (8 patients, 24.4%; HR 0.24; 95% CI 0.05–1.13; p=0.071). All-cause mortality was low and comparable (2 vs 3 patients).
Significantly, the nutritional intervention produced marked improvements in nutritional status as measured by MNA scores (+4.12 in intervention vs. −1.15 decline in controls; p<0.001) after 12 months. Correspondingly, anthropometric markers including body mass index, tricipital skinfold thickness, and arm circumference increased significantly in the intervention group. Serum albumin levels, a biochemical indicator of nutritional and inflammatory status, also improved.
Functional capacity, an important predictor of morbidity and mortality in HF, showed favorable gains: the intervention group increased their 6MWT distance by 31.3 meters at 12 months (p=0.002), whereas the control group did not experience significant change. This improvement suggests enhanced exercise tolerance linked to better nutritional status.
Expert Commentary
The PACMAN-HF subanalysis underscores the clinical importance of identifying and managing malnutrition risk in chronic HF patients. While the nutritional intervention did not achieve statistically significant reduction in mortality or hospitalizations—possibly due to limited sample size and statistical power—the observed trends and pronounced enhancements in functional capacity and nutritional metrics are clinically meaningful.
Malnutrition in HF is associated with muscle wasting, diminished immune function, and poorer cardiovascular reserve. By improving nutritional parameters, patients may gain resilience and quality of life benefits even without immediate drastic reductions in hard clinical endpoints. The findings align with recent HF guidelines advocating for comprehensive, multidisciplinary patient management that integrates nutritional assessment and intervention.
Study limitations include the relatively small sample size and the imbalance in hypertension prevalence, which might influence outcomes. Larger-scale trials are warranted to confirm potential survival benefits and to clarify the mechanistic pathways by which nutrition modulates HF progression.
Conclusions
This prespecified subanalysis of the PACMAN-HF trial demonstrated that a structured, individualized nutritional intervention in chronic HF patients at risk of malnutrition significantly improved nutritional status and functional capacity over a 12-month period. Although major clinical endpoints such as all-cause mortality and HF hospitalizations were not significantly affected, trends suggest potential benefits that merit further investigation. Incorporating nutritional screening and targeted intervention into routine HF care could enhance patient-centered outcomes and deserves consideration in clinical practice and future research frameworks.
References
Ortiz-Cortés C, Rey-Sánchez P, Gómez-Turégano P, Bover-Freire R, Calderón-García JF, Gómez-Barrado JJ, Rico-Martín S. Effectiveness of a Nutritional Intervention in Patients with Chronic Heart Failure at Risk of Malnutrition: A Prespecified Subanalysis of the PACMAN-HF Trial. Nutrients. 2025 Sep 8;17(17):2899. doi: 10.3390/nu17172899 IF: 5.0 Q1 . PMID: 40944287 IF: 5.0 Q1 ; PMCID: PMC12430209 IF: 5.0 Q1 .
Additional relevant literature:
-Dewey FE, et al. Nutrition and heart failure: Rationale and potential therapeutic perspectives. J Card Fail. 2016;22(8):670-6.
-Anker SD, et al. Nutritional interventions for heart failure patients: Current and emerging evidence. ESC Heart Fail. 2021;8(5):3772-3782.



