Highlight
- Individuals with metabolic syndrome have a 39% increased risk of developing Parkinson’s disease (PD) compared to those without the syndrome.
- Genetic predisposition amplifies PD risk in patients with metabolic syndrome, with nearly double the risk observed in high-risk genotypes.
- The PD risk increases in a dose-dependent manner according to the number of metabolic risk factors present.
- Findings emphasize the potential of lifestyle interventions targeting metabolic health to reduce PD risk, even for genetically predisposed individuals.
Study Background and Disease Burden
Parkinson’s disease is a progressive neurodegenerative disorder characterized primarily by motor dysfunction and non-motor symptoms, affecting millions worldwide. Given its incurable nature and growing incidence with aging populations, identifying modifiable risk factors is paramount. Metabolic syndrome—a constellation of metabolic abnormalities including central obesity, hypertension, dyslipidemia, and impaired glucose regulation—affects approximately one-third of adults in the US and is a known contributor to several chronic disorders such as type 2 diabetes and dementia. However, the relationship between metabolic syndrome and the risk of Parkinson’s disease has been inconclusive due to limitations in prior studies, which often had small cohorts or short follow-up periods. Given the high prevalence of metabolic syndrome and its modifiability, understanding its impact on PD risk is critical for preventive strategies and clinical management.
Study Design
The study was a large-scale, population-based longitudinal cohort analysis leveraging data from the UK Biobank. The investigators followed 467,200 individuals aged 37 to 73 years (mean age 56.5 years; 54% women) who were free of Parkinson’s disease at baseline, over a median of 15 years. Metabolic syndrome was defined according to established criteria, requiring the presence of three or more of the following: excess abdominal fat, high blood pressure, dyslipidemia (including low HDL cholesterol and elevated triglycerides), and hyperglycemia. Genetic susceptibility to PD was quantified using a polygenic risk score based on known PD-associated variants. The primary endpoint was incident Parkinson’s disease, identified through medical records and registries. Cox proportional hazards models adjusted for multiple covariates—including age, lifestyle factors, and genetic risk—were used to estimate the hazard ratios (HRs) for PD associated with metabolic syndrome and its individual components. Sensitivity analyses further adjusted for body mass index (BMI) and excluded participants with likely undiagnosed PD to validate the robustness of findings. Additionally, a meta-analysis of nine studies encompassing nearly 25 million individuals and over 98,000 PD cases was conducted to corroborate the cohort study results.
Key Findings
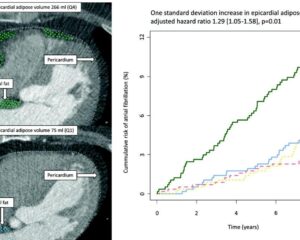
During the follow-up, 3,222 participants developed Parkinson’s disease. After comprehensive adjustment, metabolic syndrome was associated with a significant 39% increase in PD risk (HR 1.39; 95% CI 1.11-1.74). Importantly, the risk showed a dose-response relationship, with a 14% increase in PD risk per additional metabolic risk factor (P for trend = 0.001). Individuals exhibiting all five metabolic abnormalities had the highest risk among the cohort.
Breaking down individual components, excess abdominal fat conferred a 33% heightened PD risk, low HDL cholesterol a 43% higher risk, and hyperglycemia a 28% increased risk. These findings highlight the heterogeneity in contributions of different metabolic abnormalities to PD development.
Genetic predisposition markedly modified this association. Participants with both metabolic syndrome and a high polygenic PD risk score had an almost two-fold increased risk of PD compared to those with metabolic syndrome but low genetic risk (HR 1.69; P < 0.001), indicating synergistic effects between genetic susceptibility and metabolic dysfunction.
Sensitivity analyses confirmed the stability of these associations after adjusting for BMI and excluding cases of probable preclinical PD.
The meta-analysis provided additional support, revealing consistent positive associations between metabolic syndrome and PD incidence across diverse populations.
Expert Commentary
Dr. Jiao Wang, PhD, from the Karolinska Institute, emphasized the clinical implications, stating that metabolic health assessment should be integrated into a comprehensive brain health strategy. For patients with metabolic syndrome—particularly those with known genetic risk factors—more diligent neurological monitoring may facilitate earlier detection and intervention.
Neurologist Dr. Jori Fleisher of Rush University commented that this study strengthens the evidence that targeting metabolic syndrome with lifestyle modifications and clinical management could potentially alter PD risk trajectories. She noted that many patients inquire about modifiable factors influencing their disease course, and this data provides a tangible basis for intervention.
Biological plausibility for these findings stems from shared pathophysiological pathways. Metabolic syndrome is associated with systemic inflammation, oxidative stress, and mitochondrial dysfunction—mechanisms implicated in Parkinson’s neurodegeneration. Insulin resistance and dyslipidemia may also affect dopaminergic neuronal survival and brain energy metabolism.
Nevertheless, limitations should be noted. The study population predominantly comprised White individuals with possibly better baseline health, potentially limiting extrapolation to more diverse or less healthy populations. Early asymptomatic PD cases might have been missed though sensitivity analyses attempted to address this. Future research should explore mechanistic pathways and evaluate intervention efficacy in reducing PD risk.
Conclusion
This extensive cohort study and meta-analysis elucidate metabolic syndrome as a significant, modifiable risk factor for Parkinson’s disease with a substantial dose-dependent effect. The interplay between metabolic abnormalities and genetic predisposition underscores the need for personalized risk assessment and integrated management approaches targeting metabolic health. Clinicians should consider screening for metabolic syndrome in middle-aged and older adults as part of neurological risk stratification, alongside encouraging lifestyle changes including diet, exercise, and weight management. These findings advance our understanding of PD etiology and support preventive strategies that may help reduce the global burden of Parkinson’s disease.
References
Zhang X, Wang J, Dove A, Yu T, Li Q, Gottesman RF, Xu W. Metabolic Syndrome and Incidence of Parkinson Disease: A Community-Based Longitudinal Study and Meta-Analysis. Neurology. 2025 Sep 23;105(6):e214033. doi: 10.1212/WNL.0000000000214033. Epub 2025 Aug 20. PMID: 40834329; PMCID: PMC12367420.
Additional literature for mechanistic insights:
1. Kalia LV, Lang AE. Parkinson’s disease. Lancet. 2015 Aug 29;386(9996):896-912.
2. De Pablo-Fernandez E, et al. Metabolic syndrome and cognitive decline: The need for multi-domain lifestyle intervention. Ageing Res Rev. 2020 Nov;64:101176.
3. Heneka MT, et al. Neuroinflammation in Alzheimer’s Disease. Lancet Neurol. 2015 Apr;14(4):388-405.