Highlight
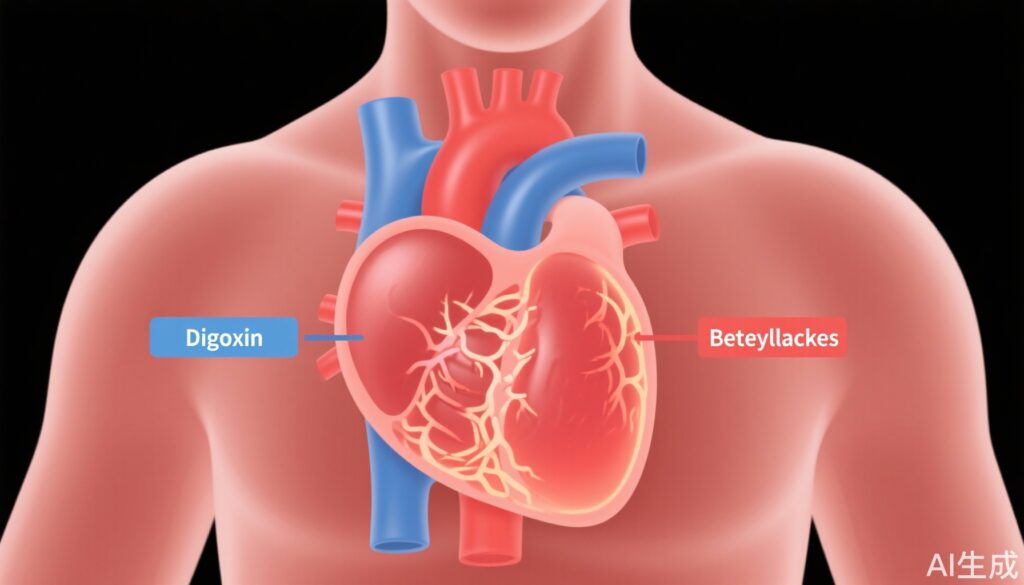
– Low-dose digoxin improves left ventricular systolic function in heart failure patients with preserved ejection fraction (LVEF ≥50%) and permanent atrial fibrillation (AF).
– Compared to beta-blockers, digoxin improves clinical symptoms, reduces NT-proBNP levels, and is associated with fewer adverse events.
– No significant improvement in systolic or diastolic function observed in patients with reduced or mid-range LVEF.
Study Background and Disease Burden
Heart failure with preserved ejection fraction (HFpEF) and concurrent permanent atrial fibrillation (AF) represent a significant clinical challenge due to complex hemodynamic alterations and limited evidence-based therapies. HFpEF accounts for approximately half of heart failure cases and poses a high risk of morbidity and hospitalization, especially in elderly populations who often have comorbid AF. Controlling heart rate and improving cardiac function remain therapeutic goals, yet optimal pharmacologic strategies for patients with permanent AF and HFpEF are not clearly established. Beta-blockers have been widely used to control heart rate in AF, but their impact on left ventricular (LV) function in this group is uncertain. Digoxin, a cardiac glycoside, exerts positive inotropic and rate-controlling effects; however, contemporary high-quality randomized data on its efficacy and safety in this population are limited. The RATE-AF randomized trial aimed to address this knowledge gap by comparing low-dose digoxin with beta-blockers in patients with permanent AF and heart failure symptoms across the LVEF spectrum.
Study Design
The RAte control Therapy Evaluation in Permanent Atrial Fibrillation (RATE-AF) trial was a randomized, controlled, assessor-blinded study enrolling patients with permanent AF and symptomatic heart failure. A total of 145 patients completed 12-month follow-up with a median age of 75 years, 44% female. Patients were allocated to receive either low-dose digoxin or beta-blockers. The primary investigative focus was on changes in left ventricular systolic and diastolic function over 12 months, evaluated by blinded echocardiography using a standardized imaging protocol and the index-beat approach. Echocardiographic parameters included left ventricular ejection fraction (LVEF), peak systolic mitral annular velocity (s’), stroke volume, global longitudinal strain, and diastolic function indices. Secondary endpoints encompassed biomarker assessment (N-terminal pro-B-type natriuretic peptide [NT-proBNP]), functional status measured by New York Heart Association (NYHA) class, arrhythmia symptom burden quantified by a modified European Heart Rhythm Association (EHRA) score, and safety outcomes including adverse event rates. Analyses were stratified by baseline LVEF categories (≥50%, 40-49%, and <40%).
Key Findings
Among the 119 patients with preserved LVEF (≥50%) at baseline, treatment with low-dose digoxin was associated with a statistically significant and clinically meaningful improvement in systolic function relative to beta-blockers. Specifically, adjusted mean increases in LVEF were 2.3% (95% CI 0.3 to 4.2; p=0.021), mitral annular s’ velocity increased by 1.1 cm/s (95% CI 1.0 to 1.2; p=0.001), and stroke volume improved by 6.5 ml (95% CI 0.4 to 12.6; p=0.037). Global longitudinal strain and diastolic parameters showed no significant differences between groups, indicating that the primary benefit was in systolic enhancement rather than diastolic function modification. Patients with mid-range (40-49%) or reduced (<40%) LVEF did not demonstrate significant differences in echocardiographic outcomes between treatments.
Importantly, digoxin therapy resulted in a significant reduction in NT-proBNP levels compared with beta-blockers (geometric mean difference 0.77; 95% CI 0.64 to 0.92; p=0.004), which reflects lower myocardial wall stress and improved cardiac load. Clinically, the odds of improvement in NYHA functional class were markedly higher with digoxin (OR 11.3, 95% CI 4.3 to 29.8; p<0.001) as were odds of better arrhythmia symptom class by modified EHRA scoring (OR 4.91, 95% CI 2.36 to 10.23; p<0.001).
Safety analyses favored digoxin, which was associated with substantially fewer adverse events (incident rate ratio 0.21, 95% CI 0.13 to 0.31; p<0.001) compared to beta-blockers. Notably, there were no significant interactions between treatment effects and baseline LVEF on these clinical and biomarker outcomes.
Expert Commentary
The RATE-AF trial offers compelling evidence supporting the use of low-dose digoxin to improve systolic performance and symptom burden in patients with permanent AF and HFpEF, a population with a rising prevalence and limited therapeutic options. The observed increments in LVEF and s’ velocity, though modest, are clinically relevant improvements in a cohort typically characterized by preserved systolic performance. These findings challenge the traditional view relegating digoxin primarily to rate control and suggest a potential role in enhancing contractile function without adverse effects on diastolic parameters.
Safety profiles in the study underscore the feasibility of low-dose digoxin as a well-tolerated alternative to beta-blockers, which may have deleterious negative inotropic effects or cause fatigue and hypotension in elderly patients. The biomarker improvements align with pathophysiological expectations of improved cardiac efficiency and reduced neurohormonal activation.
Limitations include the relatively small sample size and the absence of longer-term outcome data such as hospitalization or mortality rates. Also, contemporary HFpEF management increasingly integrates interventions targeting comorbidities and sodium–glucose cotransporter 2 inhibitors, raising questions about interaction effects. Nonetheless, RATE-AF’s robust methodology, including blinded echocardiographic assessment and adherence to a predefined imaging protocol, enhances confidence in the findings.
Conclusion
The RATE-AF randomized trial provides high-quality evidence that low-dose digoxin improves left ventricular systolic function and clinical symptoms in patients with heart failure symptoms, preserved ejection fraction, and permanent atrial fibrillation when compared with beta-blockers. The findings highlight digoxin’s dual benefit on cardiac performance and symptom relief, with an improved safety profile, advocating for reconsideration of digoxin’s therapeutic role in this challenging clinical subgroup. Further large-scale studies addressing long-term clinical outcomes and interactions with current HFpEF regimens are warranted to optimize management strategies.
References
1. Bunting KV, Champsi A, Gill SK, Saadeh K, Camm AJ, Stanbury M, Haynes S, Townend JN, Steeds RP, Kotecha D; on behalf of the RAte control Therapy Evaluation in Permanent Atrial Fibrillation (RATE‐AF) Trial Group. Low-dose digoxin improves cardiac function in patients with heart failure, preserved ejection fraction and atrial fibrillation – the RATE-AF randomized trial. Eur J Heart Fail. 2025 Sep 2. doi: 10.1002/ejhf.70022. Epub ahead of print. PMID: 40891341.
2. Paulus WJ, Tschope C, Sanderson JE, et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J. 2019;40(40):3297-3317.
3. McMurray JJV, Packer M, Desai AS, et al. Angiotensin–Neprilysin Inhibition versus Enalapril in Heart Failure. N Engl J Med. 2014;371(11):993-1004.
4. Kotecha D, Lam CSP, Van Veldhuisen DJ, Endorsed by the Heart Failure Association of the ESC. Heart Failure With Preserved Ejection Fraction and Atrial Fibrillation: Vicious Twins. J Am Coll Cardiol. 2016;68(5):439-451.
5. Zannad F, Ferreira JP, Pocock SJ, et al. SGLT2 inhibitors in patients with heart failure: a comprehensive meta-analysis of five randomised controlled trials. The Lancet. 2020;396(10254):819-829.