Study Background
Primary biliary cholangitis (PBC) is a chronic autoimmune liver disease characterized by progressive destruction of intrahepatic bile ducts leading to cholestasis, fibrosis, and potentially cirrhosis and liver failure. Ursodeoxycholic acid (UDCA) is the standard first-line treatment; however, a significant subset of patients exhibits inadequate biochemical response, necessitating second-line therapies. Obeticholic acid (OCA), a farnesoid X receptor agonist, was conditionally approved to improve outcomes in UDCA non-responders or intolerant patients. Despite promising results from initial clinical trials, including the POISE study, concerns remain about OCA’s efficacy in reducing long-term liver-related clinical events and its safety profile, notably pruritus and use in cirrhotic populations. Regulatory actions like the European Medicines Agency’s (EMA) withdrawal of marketing authorization underscore the need for further real-world evidence.
Study Design
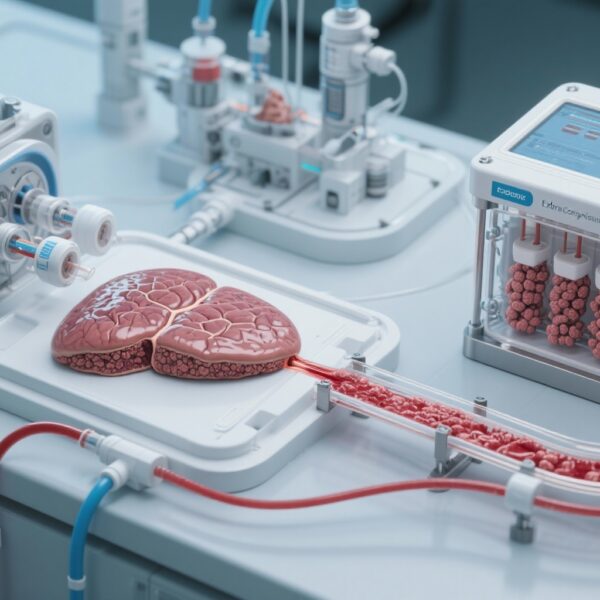
The RECAPITULATE project is a multicenter observational study leveraging data from 66 Italian centers participating in the “Italian PBC registry” and the “Club Epatologi Ospedalieri” PBC working group. This large cohort included 747 patients treated with OCA with a median follow-up period of 24 months (interquartile range 12-42 months). Patient demographics included a predominance of females (88%) with a mean age of 58 years; 28% had cirrhosis, and 14% had autoimmune hepatitis/PBC overlap syndrome. Effectiveness was assessed by biochemical response using standard POISE and normalized liver enzyme criteria, including alkaline phosphatase (ALP), alanine aminotransferase (ALT), and bilirubin within normal ranges. Safety was evaluated through the incidence and severity of de novo or worsening pruritus and discontinuation rates and their causes. Liver stiffness measurement (LSM) data, derived from elastography, were available for about 77% of the cohort, with longitudinal data for 255 patients to assess fibrosis dynamics.
Key Findings
Effectiveness
Over the follow-up period, biochemical responses improved progressively. The probability of achieving a POISE-defined response increased to 57%, and normalization of liver enzymes occurred in 20% by the 42nd month of treatment. Patients with cirrhosis had significantly lower response rates (p=0.02 for POISE and p=0.004 for normal range criteria), suggesting more advanced disease may limit biochemical improvement. Conversely, patients with the autoimmune hepatitis/PBC overlap syndrome had similar biochemical outcomes compared to pure PBC cases (p=0.8), indicating OCA’s consistent efficacy across these subgroups.
Liver Stiffness Dynamics
Liver stiffness measurement, a noninvasive surrogate for fibrosis, revealed differential patterns based on biochemical response status. Responders to OCA treatment showed a mean annual reduction in LSM of -0.48 kPa/year (95% CI -0.78 to -0.19), indicating fibrosis regression or stabilization. In contrast, non-responders experienced a slight increase in stiffness (+0.33 kPa/year; 95% CI -0.07 to 0.73), suggestive of ongoing disease progression (p<0.001 comparing groups). These findings underscore the utility of LSM as both a biomarker for treatment response and a possible predictor of clinical outcomes.
Safety and Tolerability
Seventeen percent of patients discontinued OCA during follow-up. The most common cause of discontinuation was pruritus (36.9%), consistent with known side effects of OCA, followed by discontinuation due to hepatic events (28.5%), particularly in those with cirrhosis. Patients with cirrhosis had significantly higher discontinuation rates (p<0.001), highlighting the need for close monitoring and careful patient selection in this subgroup. The study did not report unexpected safety signals beyond those established in prior clinical trials.
Expert Commentary
This expansive real-world dataset confirms that OCA maintains its biochemical efficacy and safety profile beyond controlled trial settings and over extended periods up to three and a half years. The observation that fibrosis dynamics, as measured by LSM, improve in biochemical responders lends mechanistic plausibility and supports the hypothesis that OCA may modify disease progression. The differential efficacy and safety in cirrhotic patients emphasize the necessity for individualized risk-benefit assessments. Although the EMA’s marketing authorization revocation reflects concerns about hard clinical endpoints not being adequately met in prior studies, these new findings provide important context that real-world patient populations—including those with more complex disease phenotypes—might derive meaningful benefit.
Limitations include observational design, lack of a control group, and potential confounding factors inherent to registry studies. Furthermore, the correlation between LSM changes and long-term clinical outcomes warrants further prospective validation. Despite these caveats, the large sample size and multicenter collaboration enhance the generalizability of findings across diverse clinical settings.
Conclusion
This landmark Italian multicenter real-world study affirms that obeticholic acid offers sustained biochemical efficacy and manageable safety over medium-to-long-term treatment in PBC patients. Biochemical response is closely associated with favorable liver stiffness evolution, suggesting fibrosis modification potential. Special consideration should be given to patients with cirrhosis due to lower response rates and higher discontinuation risks. These insights inform clinical decision-making, contribute to ongoing regulatory and scientific discourse, and underscore the importance of real-world evidence to complement data from randomized trials in the complex management of PBC.
Funding and Clinicaltrials.gov
Details regarding funding sources or clinical trial registrations for the RECAPITULATE project are not specified within the current dataset.
References
- Terracciani F, De Vincentis A, D’Amato D; “Italian PBC registry” and the “Club Epatologi Ospedalieri” PBC working group. Long-term effectiveness, safety, and liver stiffness dynamics of PBC treatment with obeticholic acid in real-world. JHEP Rep. 2025 May 27;7(8):101448. doi:10.1016/j.jhepr.2025.101448.
- Nevens F, Andreone P, Mazzella G, et al. A Placebo-Controlled Trial of Obeticholic Acid in Primary Biliary Cholangitis. N Engl J Med. 2016;375:631-43. doi:10.1056/NEJMoa1509840.
- European Medicines Agency. Withdrawal of the marketing authorisation for Ocaliva (obeticholic acid). 2023.
- European Association for the Study of the Liver (EASL). Clinical Practice Guidelines: Primary Biliary Cholangitis. J Hepatol. 2017;67(1):145-172.