Highlight
Liver resection after initial atezolizumab plus bevacizumab (atezo/bev) induction significantly extends time to treatment failure in patients with locally advanced hepatocellular carcinoma (HCC) without extrahepatic metastases. This phase 3 TALENTop trial interim analysis demonstrates a 40% reduction in risk of treatment failure compared to continued systemic therapy alone. The surgical approach following disease control with atezo/bev is feasible with manageable safety, and shows a trend toward improved overall survival.
Study Background
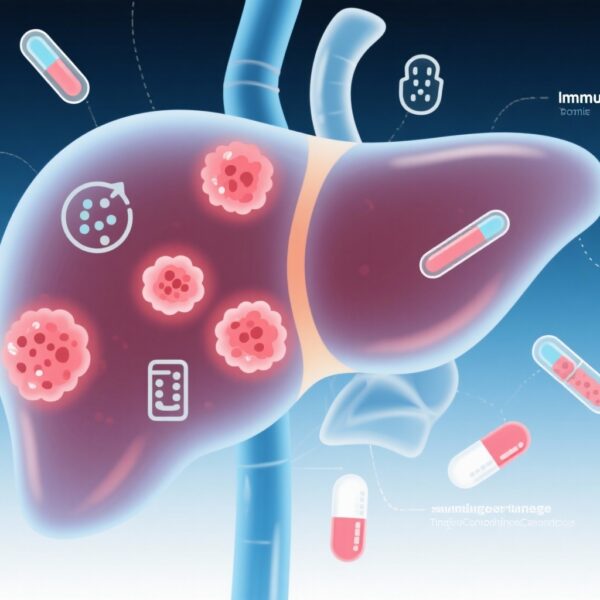
Hepatocellular carcinoma is a major global health burden, often diagnosed at advanced stages limiting curative options. For locally advanced HCC with vascular invasion but no distant metastasis, systemic therapies like the combination of atezolizumab (a PD-L1 inhibitor) plus bevacizumab (an anti-VEGF antibody) have become standard first-line treatments, offering meaningful survival benefits. However, the role of liver resection following initial systemic treatment response remains controversial. Surgery traditionally is considered for early-stage disease, but advancements in systemic therapy have opened potential for multimodal treatments aiming for enhanced disease control in select patients.
Study Design
The TALENTop trial (NCT04649489) is an ongoing, multicenter, open-label, randomized phase 3 study evaluating efficacy and safety of liver resection combined with perioperative atezolizumab plus bevacizumab against continued systemic therapy alone in patients with locally advanced HCC (vascular invasion, no extrahepatic metastases) who achieved disease control after induction therapy. Eligible treatment-naïve patients first underwent induction with three cycles of atezolizumab plus bevacizumab followed by one cycle of atezolizumab alone. Patients achieving partial response (PR) or stable disease (SD) were randomized (1:1) to either liver resection followed by one year of atezo/bev or to continue systemic therapy until progression or toxicity.
The primary endpoint was time to treatment failure (TTF), defined as time from randomization to local recurrence, progression, distant spread, or death, assessed by independent review per RECIST v1.1. Secondary endpoints included overall survival (OS) and safety assessments.
Key Findings
Out of 489 patients treated with induction therapy, 201 met criteria for randomization: 101 to surgery plus continued atezo/bev and 100 to continued atezo/bev alone. After a median follow-up of 18.4 months, the median TTF was significantly longer in the resection arm at 20.4 months versus 11.8 months in the continued therapy arm (HR 0.60; 95% CI 0.39–0.91; P=0.015). This represents a 40% reduction in the risk of treatment failure with surgery.
There was a trend toward improved OS in the resection group (HR 0.67; 95% CI 0.35–1.29), but these data are immature due to limited events (15 vs 23 deaths). Safety profile showed grade ≥3 atezo/bev–related adverse events in 27.7% of surgical patients versus 21.0% of those on systemic therapy alone. Surgical complications of grade ≥3 occurred in 21.7% of resected patients, indicating acceptable but notable perioperative risks.
Expert Commentary
These interim results address an important clinical question regarding the integration of surgery in advanced HCC management post systemic therapy response. Dr. Hui-Chuan Sun and collaborators highlight the emerging utility of liver resection in patients achieving disease stability with atezo/bev. The significant prolongation of TTF supports that surgical tumor removal can consolidate local disease control. Although OS improvement was not statistically confirmed at this interim, longer follow-up may clarify survival benefit.
This approach demonstrates biological plausibility: immune checkpoint inhibition combined with antiangiogenic therapy may downstage tumors and micrometastases, thus optimizing conditions for successful resection. However, patient selection is critical, as the study excluded those with extrahepatic metastases or progression after induction. The surgical complication rate warrants careful perioperative management and underscores the need for experienced multidisciplinary teams.
Limitations include the open-label design and immaturity of survival outcomes. Generalizability may depend on access to specialized surgical expertise and experience with immunotherapy combinations.
Conclusion
The TALENTop study interim findings provide compelling evidence that surgical resection after initial atezolizumab plus bevacizumab induction therapy significantly extends time to treatment failure in well-selected patients with locally advanced HCC without extrahepatic spread. This multimodal strategy offers a clinically meaningful improvement over continued systemic therapy alone and may represent a paradigm shift in managing advanced HCC. Longer-term outcomes including overall survival and quality of life assessments are awaited to confirm and refine the role of surgery in this setting.
Funding and Clinical Trials Registration
The TALENTop trial is supported as a multicenter investigator-initiated study; specific funding details were not disclosed in the interim report. The study is registered on ClinicalTrials.gov under identifier NCT04649489.
References
- European Society for Medical Oncology (ESMO) Congress 2025; October 17-21, 2025. Abstract #1469MO.
- Finn RS, Qin S, Ikeda M, et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N Engl J Med. 2020;382(20):1894-1905.
- Kudo M. Optimizing treatment options for advanced hepatocellular carcinoma. World J Gastroenterol. 2018;24(30):3413-3425.