Highlight
1. Historical lead exposure from gasoline combustion is associated with increased odds of memory impairment among older adults in the US.
2. Living near modern lead-emitting industrial facilities is linked to poorer cognitive outcomes, even with adult exposure.
3. Neuropathological studies indicate low-level lead exposure can promote brain changes characteristic of Alzheimer’s disease.
4. While dementia prevalence is rising with an aging population, declining rates may reflect historical lead emission controls.
Background
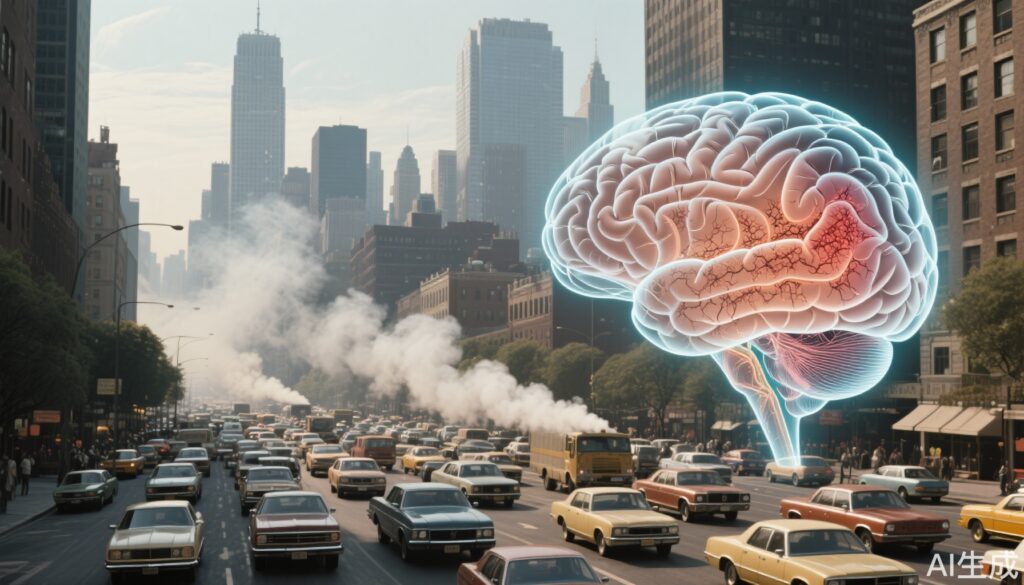
Lead, a well-known neurotoxin, was extensively used as an additive in gasoline until phased out in the 1980s and 1990s in the United States. Prior to this, children and adults, particularly in urban areas with heavy traffic, were chronically exposed to atmospheric lead. Lead exposure is linked to a range of adverse health outcomes, but its long-term impact on cognitive function and dementia risk has only recently been clarified. This is of particular relevance as the US population ages and the burden of cognitive impairment increases, even as dementia incidence rates decline.
Study Overview and Methodological Design
Three complementary studies inform the current understanding of lead’s cognitive impact:
1. The first study mapped historical airborne lead levels (HALLs) from 1960–1974 using US Environmental Protection Agency data. Geographic units called Public Use Microdata Areas (PUMAs) were analyzed, including only those with at least one lead measurement. Researchers linked these historic exposure levels to self-reported memory problems among adults aged ≥65 years who had grown up in the same PUMA, using data from the American Community Survey for two periods: 2012–2017 (n=368,208) and 2018–2021 (n=276,476). Participants were stratified by HALL into four categories (lowest, moderate, high, extremely high), and analyses were adjusted for age, sex, ethnicity, and education.
2. The second study, presented at the Alzheimer’s Association International Conference (AAIC), examined the effects of ongoing adult lead exposure. Using two harmonized cohorts (KHANDLE and STAR; n=2,409), researchers evaluated cognitive outcomes two years after measuring participants’ residential proximity to lead-emitting facilities (e.g., glass, concrete, electronics factories). Cognitive domains assessed included executive function, verbal episodic memory, and semantic memory, with a racially and ethnically diverse sample.
3. The third study presented at the AAIC explored the biological effects of low-level lead exposure in experimental settings, demonstrating increased accumulation of abnormal tau and amyloid beta in brain cells—hallmarks of Alzheimer’s disease pathology.
Key Findings
In the first study, older adults who grew up in PUMAs with moderate, high, or extremely high HALLs had significantly higher odds of reporting memory problems compared to those from areas with the lowest HALL (<0.4 μg/m3). For 2012–2017, odds ratios (OR) were 1.21 (95% CI: 1.17–1.25) for moderate and high HALL, and 1.19 (1.13–1.25) for extremely high HALL. These findings were consistent in the 2018–2021 cohort: moderate (OR 1.17), high (OR 1.20), and very high (OR 1.22).
In the second study, living within 5 km of a lead-emitting facility was associated with a 0.15 standard deviation (SD) lower episodic memory score (95% CI: -0.24 to -0.06) and a 0.20 SD lower semantic memory score (95% CI: -0.39 to -0.02) two years later. These associations were independent of age, sex, ethnicity, and socioeconomic status.
The third study’s mechanistic results suggest even low-level lead exposure can induce permanent neurobiological changes, promoting the formation of neurofibrillary tangles and amyloid plaques, both central to Alzheimer’s disease.
Mechanistic Insights and Pathophysiological Context
Lead is a potent neurotoxin that disrupts synaptic transmission, impairs neuronal cell function, and induces oxidative stress. Chronic lead exposure, especially during critical periods of brain development, may lower cognitive reserve and accelerate neurodegeneration. The observed increase in tau and amyloid pathology in experimental models provides biological plausibility for epidemiological findings linking lead to dementia. These mechanisms are consistent with prior literature indicating that early-life exposure can have persistent neurocognitive consequences decades later (Needleman, 2004; Bellinger, 2008). Lead may also potentiate vascular injury, compounding the risk for both Alzheimer’s and vascular dementia.
Clinical Implications
The findings reinforce the importance of environmental risk factor mitigation in dementia prevention strategies. For clinicians, a history of residence in high-lead areas or proximity to current lead sources should be considered when assessing cognitive risk in older adults. Historical lead exposure may account for regional disparities in cognitive aging and could influence the design of targeted screening or intervention programs. Importantly, as new disease-modifying therapies for Alzheimer’s emerge, understanding individual risk factors such as lead exposure could inform treatment stratification and prognostication.
Limitations and Controversies
Several limitations merit consideration. The reliance on self-reported memory problems may underestimate or overestimate true cognitive impairment. Retrospective exposure assessment, especially regarding residential history and environmental lead levels, introduces potential misclassification. Although analyses adjusted for key demographic factors, residual confounding cannot be excluded. Causal inference is also limited by the observational nature of these studies. Furthermore, the studies do not quantify actual blood or bone lead levels—biomarkers that would strengthen exposure assessment.
Some experts caution that while lead is a plausible risk factor, multiple environmental and socioeconomic variables may interact to shape cognitive trajectories. The generalizability of findings to populations outside the US, or to contemporary cohorts with lower lead exposure, remains to be established.
Expert Commentary or Guideline Positioning
Current guidelines from the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) recognize no safe level of lead exposure, especially in children. The accumulating evidence extends this concern to lifelong cognitive risk, underscoring the importance of primary prevention and environmental remediation. As Dr. Jennifer Brown of the study team notes, “If we understand all the risk factors, there could be different ways to stratify people for particular treatments.”
Conclusion
Decades after the phaseout of leaded gasoline, the legacy of lead exposure continues to shape cognitive health in the US. Both early-life and adult exposure are now linked to measurable cognitive impairment and potentially increased dementia risk. Ongoing surveillance, risk assessment, and environmental controls remain critical. Future research should focus on quantifying individual lead burden, elucidating gene-environment interactions, and integrating exposure history into clinical care and public health policy.
References
1. Needleman HL. Lead poisoning. Annu Rev Med. 2004;55:209-222.
2. Bellinger DC. Very low lead exposures and children’s neurodevelopment. Curr Opin Pediatr. 2008;20(2):172-7.
3. Lanphear BP, et al. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ Health Perspect. 2005;113(7):894-899.
4. United States Environmental Protection Agency. Air Quality Criteria for Lead. EPA/600/R-5/144aF. 2013.
5. Alzheimer’s Association International Conference (AAIC), 2023. Conference Abstracts.