Highlight
- Intra-arterial tenecteplase administered after successful reperfusion by thrombectomy shows tolerable safety at low doses in large vessel occlusion stroke.
- Dose escalation revealed unacceptable hemorrhagic risk at 0.1250 mg/kg, but doses 0.0313 mg/kg and 0.0625 mg/kg were safe for further study.
- Preliminary efficacy signals suggest a trend toward improved 90-day functional independence but were not statistically significant in this early-phase trial.
- Findings support progressing to larger randomized trials to clarify therapeutic benefit and optimize dosing strategies.
Study Background and Disease Burden
Large vessel occlusion (LVO) strokes account for a substantial proportion of ischemic strokes and are associated with high morbidity and mortality. Endovascular thrombectomy has revolutionized acute stroke treatment by restoring blood flow and improving clinical outcomes significantly. However, despite successful reperfusion—defined by an Extended Treatment in Cerebral Infarction (eTICI) score of 2b-3—many patients still experience poor functional recovery due to incomplete microvascular reperfusion or downstream embolization.
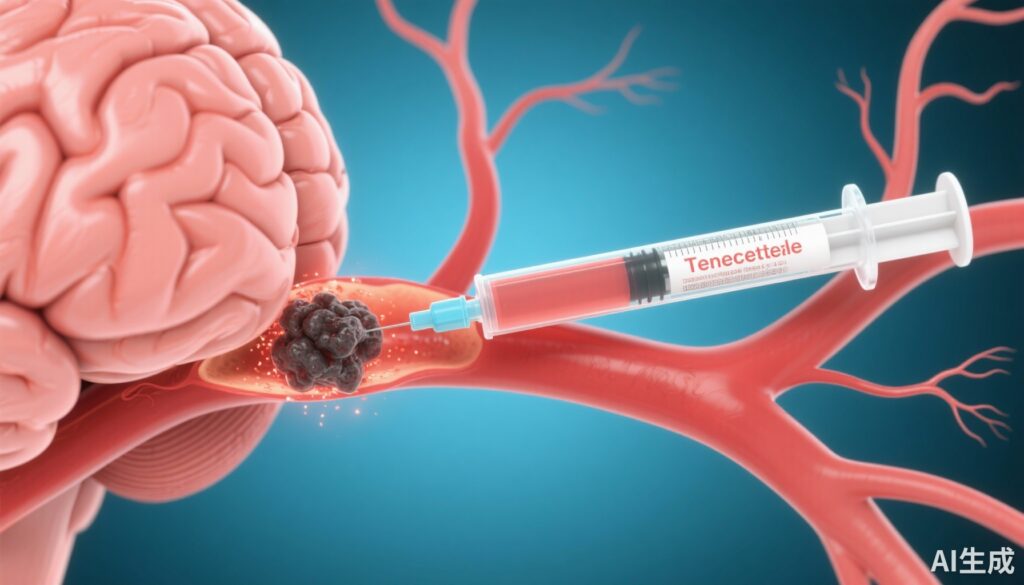
Adjunctive pharmacologic therapies aimed at enhancing reperfusion and improving microcirculatory flow post-thrombectomy remain an active area of investigation. Tenecteplase, a genetically modified tissue plasminogen activator with enhanced fibrin specificity and prolonged half-life, has shown promise as an intravenous thrombolytic in stroke. Yet, intra-arterial administration directly at the reperfused site after thrombectomy is a novel approach that may improve outcomes by targeting residual thrombus without exposing patients to systemic bleeding risk. Prior to this study, the optimal intra-arterial tenecteplase dose, its safety, and efficacy profile in this setting were undefined.
Study Design
This investigation was a multicenter, open-label trial conducted in China from 2023 through 2024, employing blinded outcome assessment to reduce bias. The trial incorporated two sequential phases:
1. Phase 1b (dose-escalation, nonrandomized): 48 patients with anterior circulation LVO and successful reperfusion within 24 hours of last known well received escalating intra-arterial tenecteplase doses (0.0313, 0.0625, 0.1250, 0.1875 mg/kg) post-thrombectomy to evaluate safety, specifically symptomatic intracranial hemorrhage (sICH) within 24 hours.
2. Phase 2a (dose-expansion, randomized): 157 eligible patients were randomized to intra-arterial tenecteplase at 0.0313 mg/kg, 0.0625 mg/kg, or control (no intra-arterial thrombolysis). The primary clinical efficacy endpoint was the proportion achieving 90-day no-disability outcome (modified Rankin Scale [mRS] score 0-1).
Eligible participants were adults with anterior circulation LVO who had attained successful reperfusion (eTICI 2b-3) through endovascular thrombectomy within the acute 24-hour treatment window.
Key Findings
Study enrollment totaled 205 patients (48 in phase 1b, 157 in phase 2a). The median age was 71 years, with a slight male predominance (55.1%).
Phase 1b Dose-Escalation Results:
– At the lowest dose (0.0313 mg/kg), 1/14 patients developed sICH.
– At 0.0625 mg/kg, 2/22 patients exhibited sICH.
– At 0.1250 mg/kg, 3/12 patients had sICH, crossing the prespecified safety threshold (P = .04), leading to halting dose escalation at this tier.
– At the highest dose (0.1875 mg/kg), safety data were limited and not prioritized due to previous tier findings.
These results identified 0.0313 mg/kg and 0.0625 mg/kg as safe doses for further assessment in phase 2a.
Phase 2a Efficacy and Safety Outcomes:
– Patients were randomized to tenecteplase 0.0313 mg/kg (n = 46), 0.0625 mg/kg (n = 46), or control (n = 65).
– The primary outcome—90-day functional independence (mRS 0-1)—occurred in 33.8% of controls, 37.0% in the 0.0313 mg/kg group (adjusted RR 0.85, 95% CI 0.54-1.35; P = .50), and 43.5% in the 0.0625 mg/kg group (adjusted RR 1.15, 95% CI 0.73-1.80; P = .55).
– No statistically significant differences in functional outcomes were observed between groups.
– Safety outcomes, including sICH and mortality, did not differ significantly among the groups.
Overall, adjunctive intra-arterial tenecteplase at 0.0313 or 0.0625 mg/kg appeared well tolerated and showed signals warranting evaluation in larger efficacy trials.
Expert Commentary
This rigorously designed, early-phase trial fills a critical knowledge gap about intra-arterial tenecteplase as an adjunct to mechanical thrombectomy in LVO stroke. The evidence identifies a safe dose range and provides preliminary efficacy data to inform phase 3 trial designs.
Experts highlight the biological rationale: tenecteplase’s fibrin-specific action could dissolve microthrombi or distal emboli left after thrombectomy, potentially improving microvascular reperfusion—a key determinant of functional recovery. The lack of significant efficacy signals in this trial may reflect limited power and sample size, as well as patient heterogeneity.
Limitations include the open-label design, relatively small sample size, and focus on anterior circulation LVO in a Chinese population, which may affect generalizability. The study’s strength lies in its methodical dose escalation and blinded outcome assessment.
Future investigations should explore optimal timing, adjunctive therapies, and mechanistic imaging correlates alongside clinical outcomes.
Conclusion
Intra-arterial tenecteplase administered immediately after successful reperfusion in anterior circulation LVO stroke is safe at doses of 0.0313 and 0.0625 mg/kg. This provides a sound basis to advance to larger randomized controlled trials to evaluate whether this approach enhances neurological recovery and long-term outcomes. Given the persistent disability associated with LVO strokes despite thrombectomy, refining adjunctive reperfusion strategies remains a priority. This study represents an important step towards personalizing stroke reperfusion therapy and optimizing post-thrombectomy care.
References
Hou X, Huang J, Wang L, He Y, Song J, Guo C, Yang S, Shi X, Chen L, Liu Q, Su J, Zeng L, Jiang M, Chen B, Cheng X, Chen S, Pan H, Shen X, Wu Y, Tang X, Wang J, Han S, Pu T, Wu C, Li F, Qu L, Fu Z, Liu H, Li Y, Mei B, Cheng Y, Hu Z, Zhang H, Lv T, Wu M, Xu R, Ye Q, Kong L, Mi S, Wu J, Wang Y, Tian Z, Sun W, Ma J, Xu X, Wu Y, Wang D, Nogueira RG, Nguyen TN, Saver JL, Zi W, Zhou Z. Intra-Arterial Tenecteplase After Successful Reperfusion in Large Vessel Occlusion Stroke: A Randomized Clinical Trial. JAMA Neurol. 2025 Sep 1;82(9):895-904. doi: 10.1001/jamaneurol.2025.2036. PMID: 40616333; PMCID: PMC12228979.