Highlight
- High-dose aumolertinib (165 mg) achieved a 12-month progression-free survival (PFS) rate of 62.1% in untreated EGFR-variant NSCLC patients with brain metastases.
- The intracranial PFS rate at 12 months reached 76.8%, indicating robust CNS activity of the drug on measurable brain lesions.
- Systemic and intracranial objective response rates (ORR) were remarkably high, exceeding 80% in both the full analysis and CNS evaluable-for-response populations.
- The safety profile was manageable; the main grade 3/4 toxicity was elevated creatine phosphokinase without any treatment-related deaths.
Study Background and Disease Burden
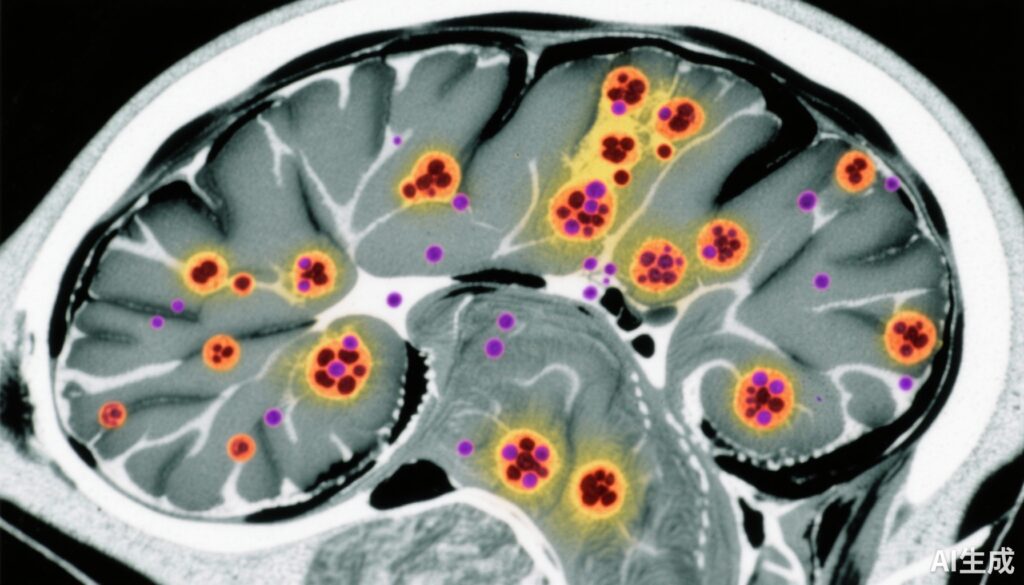
Non-small cell lung cancer (NSCLC) harboring activating mutations in the epidermal growth factor receptor (EGFR) gene represents a common lung cancer subtype, especially among East Asian populations. Despite advances in targeted therapies, central nervous system (CNS) metastases remain a formidable clinical challenge, affecting approximately 25-40% of patients with EGFR-mutant NSCLC during their disease course. Brain metastases worsen prognosis, lead to neurological morbidity, and complicate therapeutic strategies owing to the blood-brain barrier limiting drug penetration. Existing EGFR tyrosine kinase inhibitors (TKIs) like osimertinib have shown efficacy intracranially, but optimal dosing and outcomes continue to be investigated to improve survival and intracranial control.
Aumolertinib, a third-generation irreversible EGFR-TKI, has demonstrated potent systemic and CNS antitumor activity with a favorable toxicity profile. However, the efficacy and safety of high-dose aumolertinib in a frontline setting for patients with untreated EGFR-mutant NSCLC and brain metastases remained unexplored until the ACHIEVE Phase 2 clinical trial.
Study Design
This open-label, multicenter, phase 2 nonrandomized clinical trial enrolled 63 patients with untreated EGFR-mutant metastatic NSCLC accompanied by brain metastases across 10 centers in China between July 6, 2021, and August 31, 2022. Eligible patients received high-dose aumolertinib orally at 165 mg daily, continued until disease progression or unacceptable toxicity.
The primary endpoint was 12-month progression-free survival (PFS) rate, assessed by investigators per RECIST 1.1 criteria. Secondary outcomes included systemic and intracranial objective response rates (ORR), intracranial PFS, overall survival (OS), and safety. Circulating tumor DNA (ctDNA) analyses were incorporated to evaluate the prognostic significance of EGFR variant clearance.
Key Findings
With a median follow-up of 28.8 months, the trial reported compelling efficacy results. In the full analysis set of 63 patients (61.9% female; median age 60 years), the 12-month PFS rate was 62.1% (95% CI, 48.7%-73.0%), and median PFS reached 20.5 months (95% CI, 12.0-26.9). Notably, median intracranial PFS and overall survival were not reached, underscoring durable disease control.
In the subset of 49 patients with at least one measurable brain lesion, the CNS evaluable-for-response set, the 12-month intracranial PFS rate was 76.8% (95% CI, 63.2%-85.9%). Systemic ORR per RECIST 1.1 was 88.9% (56 of 63 patients) in the full cohort, with intracranial ORR of 82.5%. Within the CNS evaluable set, the ORRs were similarly high: 87.8% systemic and 85.7% intracranial. These response rates demonstrate substantial antitumor activity both systemically and within the CNS.
Safety analysis showed a manageable profile. The most frequent grade 3 or 4 treatment-related adverse event was increased blood creatine phosphokinase, occurring in 27.0% of patients (17 of 63). No treatment-related deaths were observed. Importantly, EGFR variant clearance from plasma ctDNA by day 1 of cycle 2 was independently associated with longer PFS (hazard ratio 0.14, 95% CI 0.04-0.47; P = .001), indicating a potential biomarker for early response and prognosis.
Expert Commentary
The ACHIEVE trial’s results position high-dose aumolertinib as a promising therapeutic option for EGFR-mutant NSCLC patients with brain metastases, a population with substantial unmet needs. The observed intracranial PFS and ORR rates are particularly encouraging, emphasizing the drug’s CNS penetration and efficacy—a critical consideration given the poor prognosis associated with brain metastases.
Compared to historical data with osimertinib at conventional doses, these findings suggest that higher dosing strategies may enhance intracranial control without compromising safety. However, the nonrandomized design and relatively small sample size limit direct comparisons with current standards of care. Larger randomized studies are warranted to confirm these outcomes and to evaluate long-term survival and quality of life.
The association between early ctDNA clearance of EGFR variants and improved PFS offers a valuable translational insight, potentially informing personalized treatment adaptations and early prognostication.
Conclusion
In summary, the ACHIEVE phase 2 trial demonstrates that high-dose aumolertinib (165 mg daily) confers substantial systemic and intracranial antitumor activity with a manageable safety profile in patients with untreated EGFR-mutant NSCLC and brain metastases. These data support further investigation of optimized dosing regimens of aumolertinib in this challenging clinical setting and highlight the role of plasma ctDNA as a biomarker to guide clinical decisions.
This trial adds important evidence to the evolving landscape of targeted therapies addressing CNS disease in EGFR-mutant NSCLC and offers hope for improved long-term clinical outcomes in this difficult-to-treat subgroup.