Introduction
nExposure to ambient particulate matter (PM), particularly traffic-related air pollution, has been recognized as a significant contributor to cardiovascular risk, including the elevation of blood pressure (BP), a major modifiable risk factor for morbidity and mortality worldwide. Fine particles with diameters less than 2.5 micrometers (PM2.5) and ultrafine particles (UFPs) pose particular health risks due to their ability to penetrate indoor environments and impact physiological processes. Despite the established links between PM exposure and hypertension, evidence on effective, pragmatic interventions to mitigate this risk within real-world residential settings remains limited.
Study Design and Methods
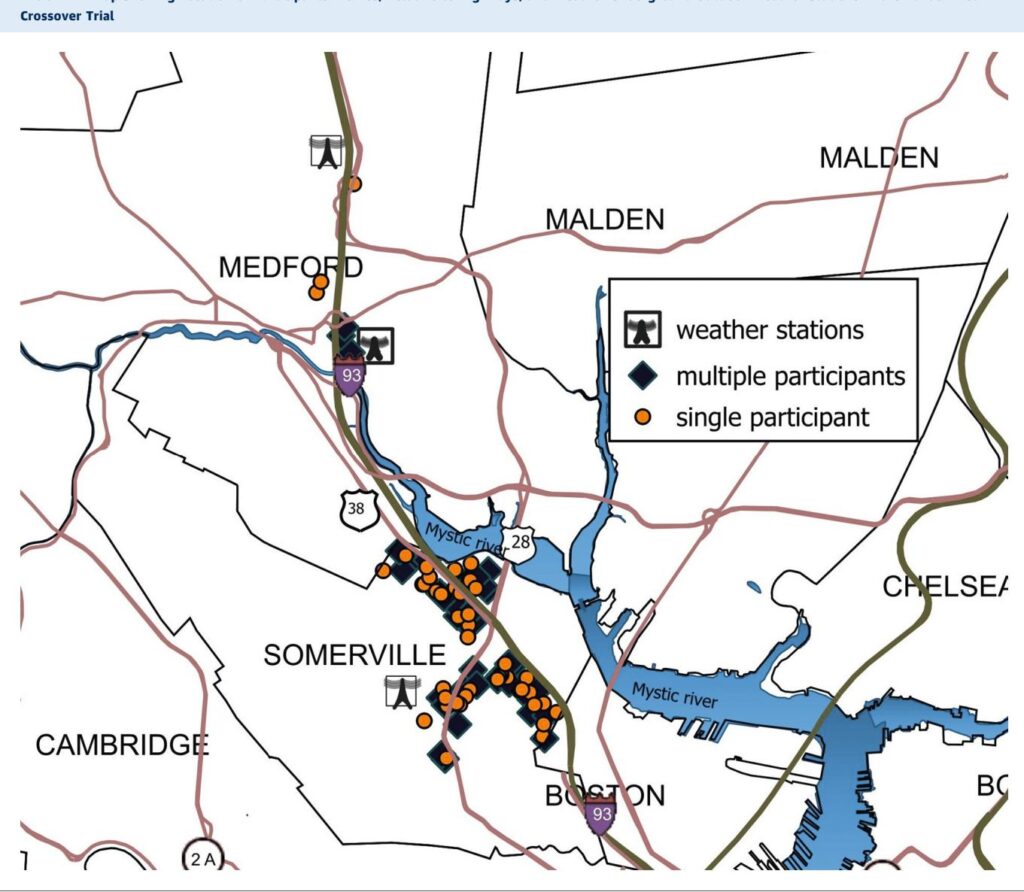
nTo address this gap, Brugge et al. conducted a pragmatic randomized, double-blinded crossover trial involving 154 adults residing within 200 meters of high-traffic highways in eastern Massachusetts, USA. The trial tested the efficacy of high-efficiency particulate arrestance (HEPA) air filtration units versus sham filtration (identical units without filters) over 1-month intervention periods separated by a 1-month washout. The study population excluded individuals on antihypertensive medications or with significant cardiovascular history to isolate the effects of PM reduction.
Participants lived their usual lifestyles without restrictions on activities, enhancing real-world applicability. Blood pressure was measured under standardized conditions using validated portable devices at the start and end of each filtration period, yielding four BP assessments per participant. A subset of residences underwent continuous indoor and outdoor PM2.5 and particle number count (PNC) monitoring to validate air purifier efficacy.
Linear mixed-effects models adjusted for potential confounders—including age, sex, baseline BP, indoor time, outdoor temperature, and perceived stress—were employed to evaluate differences in BP changes between HEPA and sham periods. Importantly, the model examined the interaction between baseline systolic BP (SBP) status (normal <120 mm Hg vs. elevated ≥120 mm Hg) and treatment effect.
Key Findings
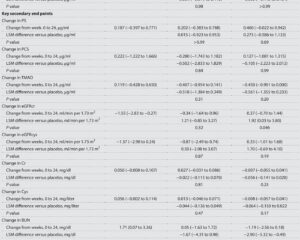
nThe filtered air environment created by HEPA purifiers yielded significant reductions in indoor PM2.5 concentrations compared to sham filtration and outdoor levels, confirming effective pollutant removal. While the overall mean SBP reduction with HEPA was modest and statistically nonsignificant (-1.1 mm Hg vs. -0.6 mm Hg sham), stratification by baseline SBP revealed a clinically meaningful effect.
Participants with elevated baseline SBP (≥120 mm Hg) experienced a significant 2.8 mm Hg reduction in SBP during HEPA filtration (p=0.03), compared to a slight nonsignificant increase during sham filtration.

This translated into a net mean difference of 3.0 mm Hg in favor of HEPA filtration (95% CI: -6.0 to -0.1, p=0.04). No significant effects on diastolic BP were observed, nor were benefits apparent in participants with normal baseline SBP.
Sensitivity analyses confirmed that the benefit magnitude increased with higher baseline SBP values, plateauing at the 120 mm Hg threshold, aligning with current clinical guidelines defining elevated BP. Exploratory analyses suggested that participants spending more time indoors might derive greater benefit, supporting the biological plausibility of indoor PM reduction impacting BP.
The study maintained robust blinding, with the James’ Blinding Index exceeding 0.8, and consistent measurement timing minimized diurnal variations as confounding factors.

Expert Commentary
nThis trial advances the growing literature linking indoor air quality improvements with cardiovascular health benefits. Unlike prior studies often confined to controlled exposure or restricted participant behavior, this pragmatic design reflects real-life conditions, bolstering generalizability.
The 3.0 mm Hg mean systolic reduction among individuals with elevated BP is clinically significant, given epidemiological data linking each 2 mm Hg SBP increase to 7-10% increased risk of ischemic heart disease and stroke mortality. Such magnitude parallels observed benefits from antihypertensive pharmacotherapy in primary prevention trials.
Mechanistically, reductions in PM exposure likely modulate autonomic nervous system activity and vascular inflammation, leading to BP improvements. However, the trial could not disentangle effects on ultrafine particles (PNC) due to measurement limitations.
Study limitations include an underrepresentation of racial/ethnic minorities and lower socioeconomic groups, in part due to exclusion criteria related to medication use. Climate and seasonal constraints (cooler months only) might limit extrapolation to hotter periods. Also, indoor temperature was not uniformly controlled, though prior evidence suggests minimal confounding.
Participant feedback highlighted practical challenges regarding air purifier noise, size, and energy consumption, which may affect long-term adherence. Future research is warranted to evaluate benefits in medicated hypertensive populations, diverse demographics, and other environmental contexts.
Conclusion
nThis trial provides compelling evidence that in-home HEPA air filtration reduces systolic blood pressure significantly among adults with elevated BP living near highways. Given the low ambient PM2.5 levels in this study setting, these findings underscore the cardiovascular benefits of air quality interventions even in relatively less polluted environments. Clinicians and public health practitioners should consider recommending HEPA air purifiers as a low-risk adjunctive measure for cardiovascular risk mitigation in vulnerable populations, particularly those with prehypertension or hypertension and residing close to major traffic corridors.
Further large-scale, diverse, and longer-term studies are needed to refine patient selection, quantify sustained benefits, and evaluate cost-effectiveness.
Reference
nBrugge D, Eliasziw M, Thanikachalam M, Kuchhal V, Morson C, Vazquez-Dodero T, Mertl A, Tallam P, Kunwar S, Sprague Martinez L, Rashid HS, Singh-Smith K, Gates H, Palma S, Goldstein-Gelb W, Ginzburg SL, Hersey SO, Majluf F, Zamore W. Effect of HEPA Filtration Air Purifiers on Blood Pressure: A Pragmatic Randomized Crossover Trial. J Am Coll Cardiol. 2025 Aug 26;86(8):577-589. doi: 10.1016/j.jacc.2025.06.037 IF: 22.3 Q1 .