Highlights
- First demonstration that haematopoietic gene therapy without cytotoxic conditioning enables sustained engraftment and clinical benefit in Fanconi anaemia-A.
- 62.5% of evaluable patients achieved the primary efficacy endpoint at two years post-infusion, with stable vector copy numbers.
- No genotoxic events or unexpected serious adverse events attributable to gene therapy were observed over long-term follow-up.
- This approach may provide a safer alternative to allogeneic transplantation for early-stage Fanconi anaemia-A.
Clinical Background and Disease Burden
Fanconi anaemia (FA) is a rare, inherited disorder characterized by progressive bone marrow failure (BMF), congenital abnormalities, and a markedly increased risk of malignancies, particularly acute myeloid leukaemia and squamous cell carcinomas. FA results from mutations in genes critical for DNA repair, with the FANCA subtype being the most common. Standard therapy for marrow failure in FA is allogeneic haematopoietic stem cell transplantation (HSCT). However, HSCT is associated with substantial risks in FA patients, including graft-versus-host disease, infections, and a significantly elevated rate of post-transplant malignancies, primarily due to the genotoxic pre-conditioning regimens required for engraftment. There is a pressing need for safer, curative therapies that avoid these complications and address the limitations of donor availability and immune compatibility.
Research Methodology
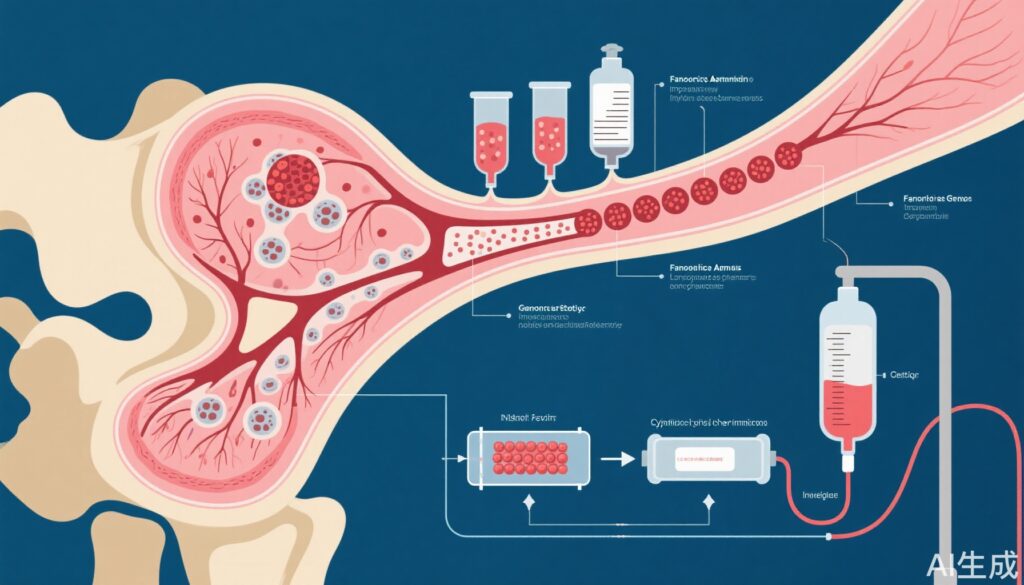
The FANCOLEN-1 study was an open-label, investigator-initiated phase 1/2 clinical trial conducted in Spain, with subsequent long-term follow-up extending up to seven years post-treatment. Nine paediatric patients with Fanconi anaemia-A in the early phase of bone marrow failure were enrolled. Peripheral blood CD34+ haematopoietic stem and progenitor cells were mobilized and collected from these patients. These cells were then transduced ex vivo using a lentiviral vector encoding a functional FANCA gene and subsequently reinfused into the patients without any cytotoxic or genotoxic conditioning regimen—an approach designed to minimize treatment-associated toxicity.
The primary efficacy endpoint was defined as the sustained engraftment of gene-corrected cells, operationalized as at least 0.1 vector copies per nucleated bone marrow or peripheral blood cell at two years post-infusion, with no significant decline from the previous year. The safety coprimary endpoint was the incidence of adverse events within the first three years post-infusion. Patients were closely monitored for both hematologic and infectious complications, vector integration, and potential genotoxicity.
Key Findings
Of the nine patients enrolled, eight received gene therapy and were evaluable for efficacy. The primary endpoint was achieved in five patients (62.5%), indicating successful and sustained engraftment of gene-corrected haematopoietic cells. The median vector copy number per nucleated cell at year two was 0.18 (IQR 0.01-0.20) in the bone marrow and 0.06 (0.01-0.19) in peripheral blood, demonstrating stable integration and persistence of the therapeutic transgene.
Importantly, no genotoxic events attributable to the lentiviral vector were detected throughout the observation period. Most treatment-emergent adverse events (TEAEs) were mild to moderate, such as transient cytopenias and common viral infections. Nine serious adverse events (grade 3-4) occurred in six patients; only one event was considered related to the infusion, and all resolved without long-term sequelae. No patient developed malignancy or clonal dominance associated with vector integration, a key safety concern in gene therapy.
Clinically, several patients demonstrated stabilization or improvement in hematologic parameters, suggesting reversal or arrest of BMF progression. This effect was achieved without the use of cytotoxic conditioning, which is typically required for allogeneic HSCT but carries significant morbidity in FA.
Mechanistic Insights and Biological Plausibility
The lentiviral vector delivers a functional FANCA gene into autologous haematopoietic stem cells, restoring the defective DNA repair pathway that underlies FA. In the absence of conditioning, the engraftment of these corrected cells relies on their selective growth advantage in the FA bone marrow environment, where endogenous stem cells are compromised by ongoing DNA damage. This unique pathophysiological context allows gene-corrected cells to expand and reconstitute hematopoiesis without the need for myeloablative therapy.
Expert Commentary
The FANCOLEN-1 trial represents a paradigm shift for treating Fanconi anaemia-A, offering a curative approach with a substantially improved safety profile. Current guidelines recognize the risks of genotoxic conditioning in FA and have highlighted the unmet need for alternative therapies. By avoiding cytotoxic preparatory regimens, this gene therapy protocol addresses a major limitation of both allogeneic transplantation and prior gene therapy attempts. The durability of engraftment and absence of genotoxicity are particularly encouraging, although longer-term surveillance for late effects remains warranted.
Controversies and Limitations
While the results are promising, several limitations should be acknowledged. The sample size is small, reflecting the rarity of the disease, and the trial was single-arm and non-randomized, precluding direct comparisons with standard HSCT. Not all patients achieved the primary endpoint, raising questions about factors influencing engraftment efficiency, such as the degree of marrow failure at baseline or stem cell mobilization efficacy. Additionally, the long-term risks of vector-related insertional mutagenesis, secondary malignancies, or clonal expansion cannot be fully excluded despite current reassuring data.
Further research is needed to optimize patient selection, vector technology, and cell processing protocols, as well as to determine the generalizability of these findings to other FA subtypes or older patients.
Conclusion
The FANCOLEN-1 phase 1/2 trial and its long-term follow-up provide the first robust evidence that autologous gene-corrected haematopoietic stem cell therapy, administered without cytotoxic conditioning, is safe and effective in early-stage Fanconi anaemia-A. This strategy offers a clinically meaningful alternative to allogeneic HSCT, significantly reducing the risk of serious complications. These findings support further development and potential adoption of gene therapy as a front-line treatment for Fanconi anaemia-A, pending larger studies and longer-term follow-up.
References
Río P, Zubicaray J, Navarro S, Gálvez E, Sánchez-Domínguez R, Nicoletti E, Sebastián E, Rothe M, Pujol R, Bogliolo M, John-Neek P, Bastone AL, Schambach A, Wang W, Schmidt M, Larcher L, Segovia JC, Yáñez RM, Alberquilla O, Díez B, Fernández-García M, García-García L, Ramírez M, Galy A, Lefrere F, Cavazzana M, Leblanc T, García de Andoin N, López-Almaraz R, Catalá A, Barquinero J, Rodríguez-Perales S, Rao G, Surrallés J, Soulier J, Díaz-de-Heredia C, Schwartz JD, Sevilla J, Bueren JA; FANCOLEN-1 gene therapy investigators. Haematopoietic gene therapy of non-conditioned patients with Fanconi anaemia-A: results from open-label phase 1/2 (FANCOLEN-1) and long-term clinical trials. Lancet. 2025 Dec 21;404(10471):2584-2592. doi: 10.1016/S0140-6736(24)01880-4
Additional relevant literature:
– Shimamura A, Alter BP. Pathophysiology and management of inherited bone marrow failure syndromes. Blood Rev. 2010;24(3):101-122.
– Dufour C, et al. Consensus guidelines for diagnosis and management of inherited bone marrow failure syndromes. Haematologica. 2015;100(1):123-136.