Introduction
Prostate cancer remains one of the most common cancers affecting men worldwide and is a major health concern, especially as men age. Despite advances in screening and treatment, understanding modifiable lifestyle factors that could reduce prostate cancer risk is a key research priority. A recent large-scale prospective cohort study led by Harvard University has shed light on a fascinating potential protective factor: frequent ejaculation. This pioneering research followed nearly 32,000 men over 18 years, revealing that men who ejaculated 21 or more times per month had a significantly lower overall risk of prostate cancer compared to those with lower ejaculation frequencies.
Scientific and Clinical Evidence: What the Data Tell Us
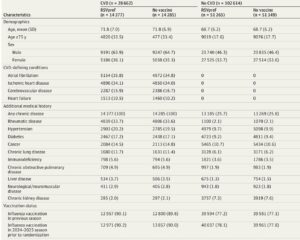
The Harvard research analyzed self-reported ejaculation frequency data from 31,925 male health professionals at three different life stages: ages 20–29, 40–49, and in the year prior to the questionnaire. These longitudinal data allowed researchers to examine the complex relationship between ejaculation frequency and prostate cancer risk over the lifespan.
Key findings include:
• Significant reduction in overall prostate cancer risk: Men reporting at least 21 ejaculations per month had a 19% lower risk of prostate cancer at ages 20–29, a 22% reduction at ages 40–49, and a 24% reduction in the year prior to questionnaire completion compared to men ejaculating 4–7 times per month.
• Impact on absolute incidence rates: Specifically, during ages 40–49, men with higher ejaculation frequency had an incidence of 6.74 cases per 1,000 person-years, compared with 8.94 per 1,000 person-years in the low-frequency group, evidencing a 2.20 per 1,000 person-years absolute reduction.
• Protection mainly against low-risk prostate cancers: The protective effect was most notable in low-risk prostate cancer cases. Men ejaculating 13 or more times monthly had a 25–28% lower risk of developing low-risk prostate cancer across all three age groups.
• Association with organ-confined and low-grade tumors: Increased ejaculation frequency correlated with lower risk of cancers localized within the prostate and of lower histological grade.
To ensure robustness, extensive sensitivity analyses were performed, including excluding cases diagnosed within 4 years of follow-up and restricting analyses to men undergoing PSA screening. The associations persisted even after adjusting for multiple confounding factors such as body mass index (BMI), physical activity, diet, smoking, alcohol consumption, family history, diabetes, and erectile dysfunction.
Interestingly, no significant association was found between ejaculation frequency and higher-risk or metastatic prostate cancers.
Understanding Potential Biological Mechanisms
The biological basis for ejaculation’s protective effect against prostate cancer is not fully understood, but several hypotheses have been proposed:
• Prostate stagnation hypothesis: Regular ejaculation may help flush out carcinogenic substances in prostatic fluid, reducing accumulation and subsequent cancer risk.
• Cellular function modulation: Frequent ejaculation might influence metabolic processes in prostate epithelial cells, preventing early carcinogenic metabolic shifts.
• Reduction of prostatic intraluminal crystals: Higher ejaculation rates may decrease crystal formation in the prostate, which has been linked to elevated cancer risk.
• Psychological and neurological influences: Increased ejaculation frequency may reduce psychological stress and inhibit central nervous system pathways that promote excessive prostate epithelial cell division.
While these mechanisms remain under investigation, the convergence of epidemiological and experimental data suggests a plausible protective role of regular ejaculation.
Limitations and Considerations
Despite its large scale and long follow-up, the study has some limitations:
• Population limitations: The cohort consisted predominantly of Caucasian male health professionals. Although biological effects of ejaculation are unlikely to vary substantially by ethnicity, replication in diverse populations remains essential.
• Potential residual confounding: Although adjustments were made for numerous lifestyle and health factors, unmeasured confounders cannot be entirely ruled out.
• Self-reporting bias: Ejaculation frequency was self-reported, and recall bias could affect accuracy.
Nonetheless, the consistency of findings across broad analyses strengthens confidence in the reported associations.
Clinical and Public Health Implications
The new evidence suggests that frequent ejaculation could be an accessible, low-cost behavior contributing to prostate cancer risk reduction. However, it is important for clinicians to present these findings within the context of overall risk management, including screening and other lifestyle factors.
Patient Scenario: What Should Men Know?
Consider “John,” a 45-year-old healthy male with a family history of prostate cancer. He is concerned about his risk and desires actionable measures to lower it. His physician discusses the Harvard study findings, emphasizing that while frequent ejaculation is associated with lower risk—particularly of less aggressive prostate cancer—it is one component of a holistic approach including diet, exercise, regular medical check-ups, and PSA screening according to current guidelines. John feels reassured that maintaining an active sexual life might provide an additional protective benefit.
Conclusion
The landmark Harvard study presents compelling evidence that men who ejaculate 21 or more times monthly across different life stages experience significantly lower overall prostate cancer risk, especially for low-risk and organ-confined tumors. Potential biological mechanisms are plausible but warrant further investigation. While the study highlights ejaculation frequency as a promising modifiable factor in prostate cancer prevention, broader research in diverse populations and mechanistic studies are needed. Clinicians can cautiously integrate these findings into patient counseling, emphasizing balanced risk reduction strategies.
References
1. Rider JR, Wilson KM, Sinnott JA, et al. Ejaculation frequency and risk of prostate cancer: updated results with an additional decade of follow-up. Eur Urol. 2016;70(6):974-982. doi:10.1016/j.eururo.2016.07.010
2. Song M, Kang D, Lee K, et al. The role of ejaculation in men’s health: A comprehensive review. Andrology. 2022;10(5):843-855. doi:10.1111/andr.13196
3. Centers for Disease Control and Prevention. Prostate Cancer Statistics. https://www.cdc.gov/cancer/prostate/statistics/index.htm
4. National Comprehensive Cancer Network (NCCN) Guidelines for Prostate Cancer Early Detection. Version 2.2024.