Highlight
1. Fontan circulatory failure (FCF) patients awaiting heart transplant face significant mortality risks both on the waitlist and within one year post-transplant.
2. Clinical cyanosis (pulse oximetry <90%) and multiple hospitalizations are independent predictors of mortality spanning waitlisting and post-transplant periods.
3. Additional factors such as hypoplastic left heart syndrome diagnosis, Fontan anatomic obstructions, and immune sensitization also contribute to post-transplant mortality.
4. Recognition of specific FCF morbidities should guide timely heart transplant referral to improve outcomes.
Study Background and Disease Burden
The Fontan procedure, a palliative surgical approach for complex single ventricle congenital heart disease, has markedly improved survival but leads to a chronic circulatory state known as Fontan circulatory failure (FCF). FCF encompasses progressive heart failure, multisystem organ dysfunction, and significant morbidity and mortality. Heart transplantation remains a critical therapy for advanced FCF; however, patient selection and timing pose significant challenges due to variable disease progression and the lack of rigorously defined clinical morbidities specific to FCF.
Understanding how specific morbidities within FCF affect outcomes before and after heart transplantation is essential to optimizing care pathways and improving survival. Prior studies have been limited by single-center design and heterogenous cohorts. This multicenter retrospective cohort study addresses these gaps by systematically analyzing FCF-specific risk factors impacting survival from the initial heart transplant waitlist through one year post-transplant.
Study Design
This retrospective cohort study involved 409 patients with Fontan palliation listed for heart transplantation between 2008 and 2022, across 20 U.S. centers. Data collected included patient demographics, detailed medical and surgical history, clinical assessments, transplant waitlist course, and peri- and post-transplant outcomes up to one year post-transplant.
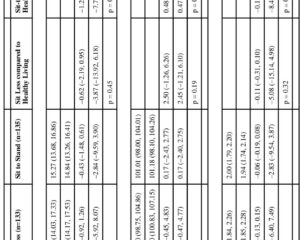
Investigators predefined FCF-specific morbidities such as aortopulmonary collateral burden, clinical cyanosis, portal variceal disease, and psychosocial factors including school/work enrollment and family structure. Univariate analyses compared characteristics between survivors and those who died either on the waitlist or within one year post-transplant. Subsequently, multivariable logistic regression identified independent predictors of mortality spanning waitlisting through the post-transplant period.
Key Findings
Among 409 waitlisted patients, 5.9% (n=24) died on the waitlist, and among the 341 patients who underwent transplant (83.4%), 8.5% (n=27) died within one year post-transplant, indicating substantial mortality burden despite advanced therapy.
Waitlist mortality risk factors (univariate): Higher aortopulmonary collateral burden; more than one hospitalization in the prior year; younger age; sleep apnea diagnosis; higher New York Heart Association (NYHA) functional class; nonenrollment in school or work; and living in single-parent homes were associated with increased risk of death before transplant.
Post-transplant 1-year mortality risk factors (univariate): Patients diagnosed with hypoplastic left heart syndrome; presence of patent fenestration; anatomic Fontan obstruction; clinical cyanosis (oxygen saturation <90%); polycythemia; portal variceal disease; mental health conditions requiring treatment; and elevated human leukocyte antigen (HLA) class II panel reactive antibody levels demonstrated higher mortality risk within the first post-transplant year.
Multivariable logistic regression demonstrated two independent predictors of mortality spanning from waitlisting to one year after transplant:
- More than one hospitalization in the year before listing (adjusted odds ratio [aOR] 2.0; 95% confidence interval [CI], 1.0–4.1; P = 0.05).
- Clinical cyanosis (aOR 5.0; 95% CI, 1.8–13.4; P = 0.002), the strongest independent predictor.
These findings underscore the critical clinical significance of hypoxemia and recent clinical instability (frequent hospitalizations) as markers for poor prognosis in Fontan patients awaiting heart transplantation.
Expert Commentary
This landmark multicenter study provides comprehensive characterization of FCF morbidities influencing survival through a critical period for single ventricle patients: waitlisting for and undergoing heart transplantation. The identification of clinical cyanosis as a potent predictor of mortality aligns with the established pathophysiology of inadequate systemic oxygen delivery exacerbating end-organ damage and complicating post-transplant recovery.
Frequent hospitalizations likely reflect decompensated heart failure or multisystem complications, advocating for early transplant evaluation when such clinical instability emerges. Additionally, immune sensitization (high HLA class II panel reactive antibodies) signals increased immunological risk post-transplant, highlighting the need for tailored immunosuppressive strategies.
While retrospective design limits causal inference, the large cohort and multi-institutional data enhance generalizability. Incorporating psychosocial factors such as education/work enrollment and single-parent home status underscores the complexity of transplant candidacy beyond pure somatic disease.
Future prospective studies should explore whether timely intervention in patients with cyanosis or increasingly frequent hospitalizations can improve transplantation success and long-term survival.
Conclusion
Fontan circulatory failure patients selected for heart transplantation face significant mortality both prior to and within one year after transplant. This study reveals that clinical cyanosis and repeated recent hospital admissions are independent, strong predictors of mortality spanning this vulnerable period. Recognition of these and other specific morbidities should prompt earlier referral and intervention to optimize transplant outcomes. Tailored clinical pathways integrating physiological, immunological, and psychosocial assessments are essential for managing this complex population. Further research is warranted to validate these findings prospectively and develop risk-stratified management strategies to improve survival and quality of life in Fontan patients requiring heart transplantation.
References
Schumacher KR, Rosenthal DN, Batazzi A, Yu S, Reichle G, Bano M, Deshpande SR, O’Connor M, Ahmed H, Chen S, Wright LK, Kindel SJ, Joong A, Ploutz M, Feingold B, Godown J, Mao CY, Lorts A, Simpson KE, Ybarra A, Richmond ME, Amdani S, Conway J, Blume ED, Cousino MK. The Impact of Fontan Circulatory Failure on Heart Transplant Survival: A 20-Center Retrospective Cohort Study. Circulation. 2025 Aug 26;152(8):508-518. doi: 10.1161/CIRCULATIONAHA.124.072961. Epub 2025 Jul 9. PMID: 40631708.