Highlight
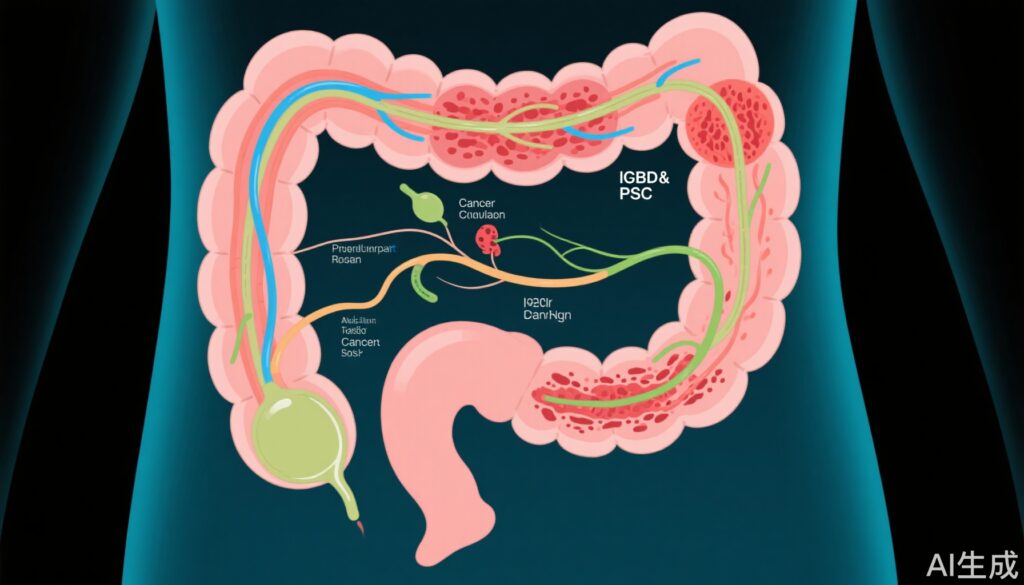
- Patients with IBD, especially those with concomitant PSC or early-onset disease, have markedly increased colorectal cancer (CRC) risk.
- CRC in IBD patients with PSC more frequently arises in the proximal colon and is associated with higher rates of synchronous tumors and mortality.
- These findings have direct implications for surveillance and surgical strategies in this high-risk population.
Background
Inflammatory bowel disease (IBD), comprising ulcerative colitis and Crohn’s disease, is a chronic relapsing inflammatory disorder of the gastrointestinal tract and is associated with an elevated risk of colorectal cancer (CRC), particularly with long-standing extensive colonic involvement. Primary sclerosing cholangitis (PSC) is a progressive cholestatic liver disease frequently coexisting with IBD, affecting approximately 2–7% of IBD patients. PSC confers a compounded risk of both hepatobiliary and colorectal malignancies, presenting a distinct clinical challenge. In light of the disease burden and the need for precise cancer prevention strategies, robust epidemiological data are critical to inform screening and management guidelines.
Study Overview and Methodological Design
The referenced study by Abdalla et al. utilized a nationwide, population-based cohort from the Swedish National Patient Register, enrolling patients diagnosed with IBD between January 1969 and December 2014. The cohort included 85,813 individuals with IBD alone and 3,066 with IBD and concomitant PSC. Each case was matched to five general population controls without IBD (n = 432,037) based on age, sex, and geography. Diagnoses of PSC were confirmed via recorded cholangitis diagnoses. Both incident CRC and cause of death were ascertained through the Swedish Cancer and Death Registers. Synchronous CRCs, defined as two or more tumors diagnosed within 180 days, were also analyzed. The study included patients who underwent colectomy, ensuring comprehensive capture of CRC risk. The primary endpoint was the incidence of CRC; secondary endpoints included location of CRC, synchronous tumors, and CRC-related mortality.
Key Findings
Patients with IBD and PSC exhibited a profoundly increased CRC incidence rate (IR) of 269/100,000 person-years compared to 95/100,000 person-years for IBD without PSC and only 58/100,000 person-years among matched controls (P < .001). The highest risk was observed in patients with unclassified IBD and PSC (IR ratio [IRR], 7.38; 95% CI, 5.56–9.63). Importantly, early-onset IBD (diagnosed before age 20) was associated with an exceptional elevation in CRC risk, particularly when co-occurring with PSC (IRR, 74.97 vs. 18.75 for IBD alone; P < .001).
CRC in IBD-PSC patients was more frequently located in the proximal colon (37.5% in caecum and ascending colon) compared to IBD without PSC (27%) and controls (22.4%). The proportion of synchronous CRCs was also higher in IBD-PSC (4.7%) and IBD alone (4.4%) than in controls (1.9%). Mortality following CRC diagnosis was highest in the IBD-PSC group (adjusted hazard ratio, 2.56; P < .001), underscoring the aggressive nature of cancer in this population.
Mechanistic Insights and Pathophysiological Context
The synergistic increase in CRC risk among IBD patients with PSC likely reflects a confluence of chronic inflammatory stimuli, altered bile acid metabolism, microbiome dysbiosis, and immunological perturbations. In PSC, chronic cholestasis and ongoing hepatobiliary inflammation may promote carcinogenic milieu throughout the colorectum, particularly the proximal segments where bile acid exposure is greatest. Early-onset IBD, associated with more extensive and aggressive colitis, further amplifies cumulative carcinogenic risk. The high prevalence of proximal and synchronous cancers in PSC underscores the field effect of inflammation and possibly genetic or epigenetic predisposition.
Clinical Implications
These findings have immediate translational relevance. First, individuals with IBD—especially those with concomitant PSC or early-onset disease—require intensified CRC surveillance, often with more frequent colonoscopy and consideration of advanced imaging or molecular screening modalities. The predilection for proximal colon involvement in IBD-PSC patients necessitates complete colonoscopic evaluation and may influence surgical decision-making. For patients requiring colectomy for dysplasia or cancer, awareness of high proximal and synchronous tumor risk should guide the extent of resection and reconstruction strategy (e.g., total proctocolectomy versus segmental resection, ileal pouch-anal anastomosis considerations). Multidisciplinary management, involving gastroenterology, hepatology, colorectal surgery, and oncology, is essential.
Limitations and Controversies
Limitations include the potential for misclassification bias due to reliance on registry data for PSC diagnosis, lack of granular information on disease phenotype (extent, severity), medication exposure, and adherence to surveillance protocols. Changes in diagnostic criteria and therapeutic strategies over the multi-decade study period may also confound risk estimates. Additionally, the Swedish population is predominantly Caucasian, possibly limiting generalizability to more diverse populations. While the absolute risk remains low in some subgroups, the relative risk is substantial, necessitating individualized risk assessment.
Expert Commentary or Guideline Positioning
Recent guidelines, including those from the American Gastroenterological Association and the European Crohn’s and Colitis Organisation, recognize PSC as a defining high-risk feature for CRC in IBD, warranting annual surveillance colonoscopy beginning at IBD diagnosis. These findings reinforce and quantify this recommendation. Dr. Peter Higgins, a leading IBD specialist, notes, “The proximity of CRC to the time of PSC diagnosis suggests that surveillance and preventive strategies must be aggressive from the outset.”
Conclusion
This comprehensive Swedish cohort study provides robust evidence that patients with IBD, especially those with PSC or early-onset disease, are at markedly increased risk for colorectal cancer—particularly in the proximal colon and with higher rates of synchronous tumors and mortality. Vigilant, tailored surveillance and multidisciplinary care are imperative. Further research is needed to refine risk stratification, explore mechanistic pathways, and optimize prevention strategies for this vulnerable population.
References
1. Abdalla M, Eberhardson M, Landerholm K, Andersson RE, Myrelid P. Impact of inflammatory bowel disease and primary sclerosing cholangitis on colorectal cancer risk: national cohort study. Clin Gastroenterol Hepatol. 2025 Jul 22:S1542-3565(25)00621-4. doi: 10.1016/j.cgh.2025.06.037.
2. Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48(4):526-535.
3. Chapman R, Fevery J, Kalloo A, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51(2):660-678.
4. Farraye FA, et al. AGA Clinical Practice Update on Colorectal Cancer Surveillance in Inflammatory Bowel Disease: Expert Review. Gastroenterology. 2017; 153(3): 822–835.