Highlight
- Elafibranor, a dual PPAR-α/δ agonist, was evaluated in a 12-week double-blind randomized-controlled trial (ELMWOOD) for patients with primary sclerosing cholangitis (PSC).
- The drug was generally well tolerated with a safety profile comparable to placebo, and serious adverse events occurred only in the placebo group.
- Significant reductions in alkaline phosphatase (ALP), a key biomarker of cholestasis, were observed with elafibranor at both 80 mg and 120 mg doses compared to placebo.
- The higher 120 mg dose produced a greater magnitude of ALP reduction and showed potential stabilization of fibrosis markers, supporting the rationale for larger, longer-term studies.
Study Background
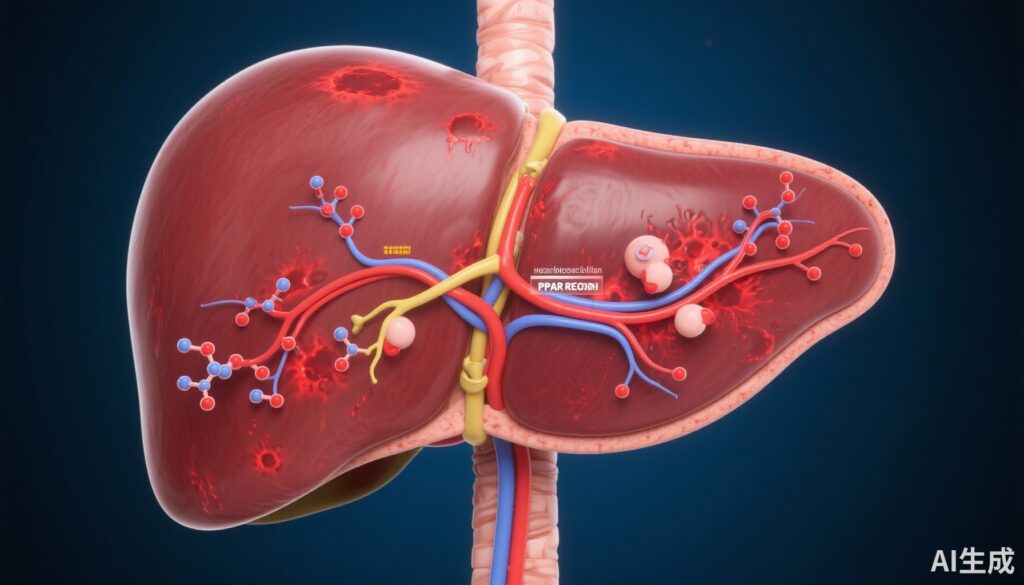
Primary sclerosing cholangitis (PSC) is a rare, chronic cholestatic liver disease characterized by progressive inflammation and fibrosis of the bile ducts, leading to liver cirrhosis, portal hypertension, and an increased risk for cholangiocarcinoma. The etiology remains incompletely understood, and there are currently no approved therapies shown to reliably halt disease progression. Ursodeoxycholic acid (UDCA) is widely used but provides limited clinical benefit in altering long-term outcomes.
The unmet need for effective, well-tolerated therapies that improve biochemical markers and potentially slow disease progression is substantial. Given the involvement of metabolic and inflammatory pathways in PSC pathogenesis, modulation of peroxisome proliferator-activated receptors (PPARs), especially the dual PPAR-α/δ agonist elafibranor, offers a promising therapeutic approach. PPAR activation influences lipid metabolism, inflammation, and fibrogenesis, key processes in PSC progression.
Study Design
The ELMWOOD trial (NCT05627362) was a multicenter, phase II, double-blind, randomized controlled study evaluating the safety and efficacy of elafibranor in adult patients with PSC and moderate elevation of alkaline phosphatase (ALP ≥1.5× upper limit of normal). A total of 68 participants were randomized into three groups: elafibranor 80 mg (n=22), elafibranor 120 mg (n=23), or placebo (n=23). The treatment period spanned 12 weeks.
Primary endpoints focused on safety and tolerability, specifically treatment-emergent adverse events (TEAEs) and discontinuation rates. Secondary endpoints included changes from baseline in ALP levels and enhanced liver fibrosis (ELF) score, a validated marker reflecting fibrosis severity.
Baseline characteristics indicated a predominantly male cohort (54.4%) with a mean age of 46.3 years; 55.9% had concomitant inflammatory bowel disease, and approximately 70% were receiving UDCA at study entry. Baseline ALP averaged 369.5 U/L, with nearly half of the participants exhibiting ELF scores above 9.8, indicative of advanced fibrosis.
Key Findings
Safety and Tolerability: Treatment-emergent adverse events were reported in 68.2% of patients receiving elafibranor 80 mg, 78.3% with 120 mg, and 69.6% with placebo. Discontinuations due to adverse events were low across all arms (4.5% in 80 mg, 4.3% in 120 mg, and 8.7% in placebo). Notably, serious TEAEs occurred only in the placebo group (4.3%), suggesting favorable tolerability of elafibranor.
Biochemical Response: Both doses of elafibranor significantly reduced ALP relative to placebo. The least squares mean (LSMean) treatment difference for ALP reduction versus placebo was -35.3% (95% CI: -49.2 to -21.4) for the 80 mg group and -54.7% (95% CI: -68.3 to -41.0) for the 120 mg group. ALP normalization occurred exclusively in the elafibranor-treated groups, at rates of 9.1% (80 mg) and 17.4% (120 mg). As ALP is a key prognostic biomarker in PSC, these reductions suggest meaningful biochemical improvement.
Fibrosis Markers: The ELF score changes trended toward improvement with elafibranor but did not reach statistical significance over this relatively short 12-week period. LSMean differences compared to placebo were -0.19 (95% CI: -0.52 to +0.15) and -0.28 (95% CI: -0.62 to +0.06) for the 80 mg and 120 mg dose groups, respectively, indicating potential early antifibrotic effects deserving further exploration in studies with longer follow-up.
Additional Observations: Preliminary data also indicated possible improvements in pruritus, a common and distressing symptom in PSC, though this requires formal assessment in future trials.
Expert Commentary
The ELMWOOD trial provides promising evidence supporting the tolerability and efficacy of elafibranor in PSC, a disease with limited therapeutic options. The biochemical improvements, particularly ALP reductions, are encouraging given their established association with clinical outcomes in PSC. The dose-dependent response further substantiates the therapeutic potential of the 120 mg dose.
The absence of serious adverse events in the elafibranor arms and comparable rates of TEAEs to placebo is notable, especially for a chronic liver disease therapy. However, limitations include the relatively short treatment duration and modest sample size, which preclude definitive conclusions on long-term clinical benefit or histological improvement.
Mechanistically, dual PPAR-α/δ activation targets several pathways central to PSC pathogenesis, including lipid metabolism, inflammation moderation, and fibrosis attenuation. These mechanistic insights align with observed biochemical benefits and support continued clinical development.
Future studies should extend treatment duration, increase participant numbers, and incorporate clinical endpoints such as progression to cirrhosis, transplantation-free survival, or patient-reported outcomes to solidify elafibranor’s role in PSC management.
Conclusion
Elafibranor demonstrates a favorable safety profile and significant biochemical efficacy in patients with primary sclerosing cholangitis, highlighting its potential as a therapeutic agent for this challenging condition. The dose-dependent ALP reductions and preliminary fibrosis marker stabilization provide a compelling rationale for larger, longer-term clinical trials to establish its impact on disease progression and patient-centered outcomes.
Funding and Trial Registration
The ELMWOOD trial was registered with ClinicalTrials.gov (NCT05627362). Detailed funding sources were not reported in the current publication.
References
Levy C, Abouda GF, Bilir BM, et al. Safety and efficacy of elafibranor in primary sclerosing cholangitis: The ELMWOOD phase II randomized-controlled trial. J Hepatol. 2025 May 8:S0168-8278(25)00252-1. doi: 10.1016/j.jhep.2025.04.025. Epub ahead of print. PMID: 40350321.