Highlight
- Three commonly recommended antihypertensive dual combination therapies were compared in a large randomized trial in India.
- All three combinations—amlodipine-perindopril, perindopril-indapamide, and amlodipine-indapamide—achieved approximately 14 mmHg reductions in ambulatory systolic BP at 6 months.
- Hypertension control rates were similar and high (~70%) across all treatment arms with minimal safety concerns.
- These data fill a critical evidence gap for optimizing combination therapy in South Asian hypertensive patients.
Study Background and Disease Burden
Hypertension represents a major public health burden worldwide, with disproportionately high prevalence and suboptimal control in South Asia, including India. This region exhibits unique risk factor profiles and often manifests hypertension at younger ages. Despite the burden, evidence guiding optimal antihypertensive dual therapy combinations in South Asian populations remains scarce. Combination therapy is recommended early in hypertension management, especially when monotherapy is insufficient to achieve blood pressure (BP) goals, but data specific to South Asians are lacking. Given the ethnic, genetic, and environmental heterogeneity impacting pharmacologic response, establishing effective, safe, and culturally adaptable dual therapies in this demographic is crucial to mitigate cardiovascular risk.
Study Design
The TOPSPIN randomized clinical trial (ClinicalTrials.gov NCT05683301) was a multicenter, single-blinded study conducted across India to evaluate three frequently used dual antihypertensive combinations: amlodipine-perindopril, perindopril-indapamide, and amlodipine-indapamide.
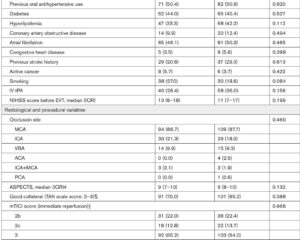
Participants were Indian adults aged 30 to 79 years (mean age 52 years; 42% female) who had either untreated sitting systolic blood pressure (SBP) of 150–179 mmHg or treated SBP of 140–159 mmHg on monotherapy. Participants were randomized 1:1:1 to receive one of the three single-pill combination therapies.
The primary endpoint was the mean change in 24-hour ambulatory systolic BP after 6 months of treatment. Secondary outcomes included mean day-time and night-time ambulatory BP, office BP measurements, and hypertension control rates defined as sitting BP <140/90 mmHg. Safety and tolerability profiles were also captured systematically.
Key Findings
From 1,981 enrolled participants, 1,637 completed valid 24-hour ambulatory BP monitoring at 6 months. All three treatment groups showed robust and clinically meaningful reductions in ambulatory and office BP measurements:
– The mean reduction in 24-hour ambulatory SBP was approximately 14 mmHg, with concurrent diastolic BP reductions around 8 mmHg across all groups.
– Office BP measurements demonstrated even larger reductions averaging 30 mmHg systolic and 14 mmHg diastolic.
– Hypertension control rates (BP <140/90 mmHg) were achieved in about 70% of participants in each treatment arm.
No statistically significant difference was observed between the groups in primary or secondary endpoints, indicating comparable efficacy among amlodipine-perindopril, perindopril-indapamide, and amlodipine-indapamide combinations.
Safety analyses revealed all combinations were well tolerated with no major adverse events or differential side effect profiles. This supports the interchangeable use of these combinations based on patient characteristics, cost, or availability.
Expert Commentary
This trial addresses an important evidence void for hypertension management tailored to Indian and broader South Asian populations. Considering pharmacodynamic and pharmacokinetic variations among ethnic groups, these findings underscore that commonly recommended dual therapies are equally effective and safe in this population subset.
The use of 24-hour ambulatory BP monitoring as the primary outcome strengthens the reliability and clinical applicability of these results, given ambulatory BP’s closer link to cardiovascular outcomes compared to office measurements alone. Achieving nearly 70% control rates is promising and aligns with contemporary hypertension guidelines advocating for early initiation of combination therapies.
Limitations include the single-blinded design, potential regional healthcare access variability, and the relatively short six-month follow-up, which precludes assessing long-term cardiovascular outcomes. Further studies incorporating diverse South Asian populations and longer-term endpoints will be valuable.
Conclusion
In conclusion, this landmark randomized clinical trial demonstrates that amlodipine-perindopril, perindopril-indapamide, and amlodipine-indapamide dual therapies are equally efficacious and safe for blood pressure control in Indian adults with hypertension. These findings provide practical guidance for clinicians in India and South Asia when selecting antihypertensive combinations, potentially improving hypertension management and reducing cardiovascular risk.
Future research should focus on cost-effectiveness analyses, patient preferences, and longer-term comparative outcomes to optimize personalized hypertension care pathways in this high-risk population.
References
1. Prabhakaran D, Roy A, Chandrasekaran AM, et al; TOPSPIN Clinical Consortia; Poulter NR. Comparison of dual therapies for hypertension treatment in India: a randomized clinical trial. Nat Med. 2025 Sep;31(9):3169-3175. doi: 10.1038/s41591-025-03854-w. Epub 2025 Jul 25. PMID: 40715816; PMCID: PMC12443627.
2. Williams B, Mancia G, Spiering W, et al. 2023 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2023;44(49):4036-4136. doi:10.1093/eurheartj/ehac592.
3. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA Hypertension Guideline. J Am Coll Cardiol. 2018;71(19):e127-e248. doi:10.1016/j.jacc.2017.11.006.