Highlights
– In a pooled European cohort (n=5,550), diabetes mellitus (DM) was associated with lower odds of abnormal amyloid beta (Aβ) and phosphorylated tau‑181 (p‑tau181) among cognitively impaired participants.
– In cognitively normal (CN) individuals without Aβ pathology, DM was associated with higher odds of total tau (t‑tau) abnormalities and medial temporal atrophy (MTA), suggesting non‑AD neurodegenerative pathways.
– Findings imply that diabetes may contribute to dementia via mechanisms distinct from classic Alzheimer’s disease (AD) pathology, highlighting the need for tailored diagnostic and preventive strategies.
Background
Dementia is a heterogeneous syndrome with multiple interacting pathogenic pathways. Type 2 diabetes mellitus (T2DM) is an established epidemiologic risk factor for cognitive decline and dementia, but the mechanisms linking diabetes to neurodegeneration remain incompletely defined. Several hypotheses are active in the field: accelerated cerebrovascular disease, promotion of Alzheimer’s disease (AD) pathology (amyloid and tau), and direct metabolic/neurodegenerative effects mediated by insulin resistance, chronic inflammation, oxidative stress, and mitochondrial dysfunction.
Clarifying whether diabetes promotes canonical AD pathology (Aβ deposition and tau phosphorylation) versus alternative neurodegenerative or vascular pathways has important implications for biomarker use, clinical prognosis, and potential targeted interventions. The published study by van Gils and colleagues pooled European aging and memory clinic cohorts to examine associations between diabetes and multimodal AD biomarkers and markers of vascular burden across the clinical spectrum from cognitively normal (CN) to mild cognitive impairment (MCI) and dementia.
Study design
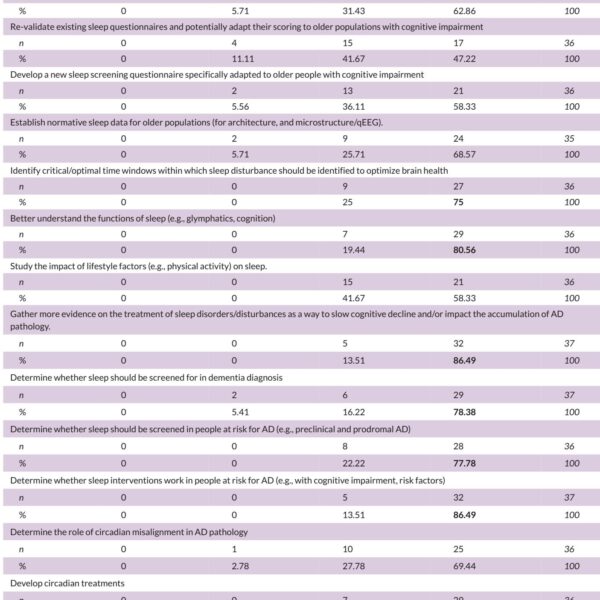
van Gils et al. performed a cross‑sectional analysis of 5,550 participants drawn from multiple European aging and memory clinic cohorts. The sample included cognitively normal individuals, those with MCI, and individuals with dementia. The principal exposures were presence of diabetes mellitus (DM) ascertained within cohort protocols. Outcomes comprised biomarker indicators of AD pathology and neurodegeneration: amyloid beta (Aβ), phosphorylated tau‑181 (p‑tau181), total tau (t‑tau), and medial temporal atrophy (MTA) assessed by neuroimaging. Vascular burden was measured by white matter hyperintensities (WMH) and cerebral microbleeds.
Primary analyses used logistic regression to estimate associations between DM and dichotomized biomarker abnormalities across diagnostic strata (CN, MCI, dementia). Secondary analyses examined combined biomarker profiles, for example Aβ status together with p‑tau181, t‑tau, MTA, WMH, or microbleeds, to identify patterns in which diabetes might differentially relate to AD pathology versus other neurodegenerative or vascular features.
Key findings
The pooled dataset included 5,550 participants with a mean age of 65.8 ± 8.7 years; 8.7% had diabetes. The principal, adjusted findings were as follows (odds ratios [OR] and 95% confidence intervals [CI] reported as in the original paper):
1) Diabetes and AD biomarkers in cognitively impaired individuals
- In participants with MCI, DM was associated with lower odds of abnormal Aβ (OR = 0.70, 95% CI 0.51–0.95; p = 0.02).
- In participants with dementia, DM was also associated with lower odds of abnormal Aβ (OR = 0.44, 95% CI 0.26–0.78; p = 0.003) and with lower odds of abnormal p‑tau181 (OR = 0.64, 95% CI 0.41–1.00; p = 0.045).
These results indicate that among clinically symptomatic individuals (MCI or dementia), diabetes was paradoxically linked to reduced probability of exhibiting canonical AD proteinopathies.
2) Diabetes and neurodegeneration in cognitively normal individuals
- In cognitively normal participants who were Aβ‑negative, diabetes was associated with higher odds of abnormal t‑tau (OR = 1.57, 95% CI 1.00–2.46; p = 0.048) and with higher odds of MTA (OR = 1.96, 95% CI 1.05–3.68; p = 0.04).
These secondary analyses suggest that in the absence of amyloid pathology, diabetes relates to biomarkers of neuronal injury and medial temporal structural change.
3) Vascular burden
The primary report focused on the AD biomarker relationships described above. There were no consistent findings reported that diabetes increased the odds of WMH or microbleeds across the diagnostic strata in the same way as the AD biomarkers; the most striking pattern was the dissociation between lower Aβ/p‑tau prevalence in diabetics with cognitive impairment versus higher neurodegeneration markers in Aβ‑negative, cognitively normal diabetics.
Interpretation and clinical implications
At face value, these results challenge a straightforward model in which diabetes uniformly accelerates AD pathology. Instead, van Gils et al. provide evidence for a more nuanced scenario:
- In persons already manifesting cognitive impairment, diabetes was associated with lower prevalence of amyloid and p‑tau pathology, implying that diabetes‑related dementia phenotypes may more often reflect non‑AD processes in these individuals.
- Among cognitively normal adults who lack amyloid pathology, diabetes was associated with markers of neuronal injury and medial temporal atrophy, which may represent early, non‑amyloid neurodegenerative changes related to metabolic dysfunction.
Collectively, the findings imply that diabetes can contribute to cognition loss through mechanisms other than canonical AD proteinopathy — for example, via metabolic neurotoxicity, insulin signaling disruption, inflammation, small‑vessel disease not fully captured by standard WMH measures, or coexisting Lewy body or other pathologies. For clinicians, the practical consequences are severalfold:
- Diagnostic evaluation of cognitive impairment in people with diabetes should not assume AD pathology; biomarker confirmation (CSF, PET, or validated blood tests) becomes particularly valuable to subtype dementia and guide prognosis and therapy.
- Prevention efforts should emphasize aggressive management of metabolic and vascular risk factors even if they do not directly reduce amyloid burden — because diabetes appears linked to other neurodegenerative pathways.
- Patients with diabetes and cognitive complaints may require monitoring for non‑AD neurodegenerative change; early structural imaging and tau/tau‑related biomarker assessments could help identify at‑risk individuals.
Expert commentary, mechanistic considerations, and limitations
Mechanistic plausibility: Experimental and clinical data support multiple routes by which diabetes may damage the brain without necessarily increasing amyloid deposition. Insulin resistance impairs neuronal glucose handling and synaptic function; chronic hyperglycemia and advanced glycation end products drive oxidative stress; and microvascular dysfunction can produce ischemic injury to medial temporal structures. Some preclinical models suggest that insulin signaling influences tau phosphorylation and clearance, but human data are mixed — consistent with the pattern observed here.
Study strengths include the large pooled sample from multiple European cohorts spanning the cognitive spectrum and the multimodal biomarker assessment strategy, which allowed interrogation of AD proteinopathies, neurodegeneration, and vascular imaging markers. The secondary profile analyses (Aβ combined with other markers) are particularly informative for etiologic heterogeneity.
Key limitations to consider:
- Cross‑sectional design: temporality cannot be established. It is unclear whether diabetes precedes the observed biomarker changes or whether shared confounders affect both diabetes and biomarker status.
- Heterogeneity across cohorts: variations in biomarker modalities (CSF vs plasma vs PET), assay thresholds, diabetes definitions, duration and severity of diabetes, glycemic control, and medication use (metformin, insulin, GLP‑1 receptor agonists) may influence associations. The pooled approach increases statistical power but can obscure cohort‑specific effects.
- Residual confounding: obesity, physical activity, socioeconomic status, and comorbidities might mediate or confound observed relationships despite statistical adjustment.
- Vascular burden measures (WMH, microbleeds) are imperfect proxies for cerebrovascular disease; other forms of small‑vessel or microinfarct pathology could be missed.
Future research directions: Longitudinal cohort studies stratified by diabetes duration, control (HbA1c), and treatment regimen are needed to map trajectories of biomarkers over time. Randomized trials of metabolic interventions (e.g., intensive glycemic control, insulin sensitizers, weight loss, GLP‑1 receptor agonists) with cognitive and biomarker endpoints would be informative. Autopsy‑based clinicopathologic correlation remains the gold standard for establishing whether diabetes increases the prevalence of non‑AD pathologies.
Conclusion
The van Gils et al. study adds important evidence that diabetes does not simply amplify Alzheimer’s proteinopathy across the board. Instead, diabetes appears associated with lower odds of Aβ and p‑tau pathology among clinically impaired individuals, while in cognitively normal, Aβ‑negative adults diabetes is linked to markers of neuronal injury and medial temporal atrophy. These results support a model in which diabetes increases dementia risk through heterogeneous pathways, often independent of classical AD pathology. Clinical practice should therefore prioritize comprehensive biomarker‑driven diagnosis and aggressive management of metabolic and vascular risks, and research should focus on longitudinal and interventional studies to delineate causal mechanisms and effective prevention strategies.
Funding and clinicaltrials.gov
Funding and trial registration details are reported in the original publication: van Gils V, Jansen WJ, van der Flier WM, et al. Alzheimers Dement. 2025;21(10):e70804. For cohort‑level funding and other administrative details, see the study’s full text and supplement.
References
1. van Gils V, Jansen WJ, van der Flier WM, Martinez‑Lage P, Hort J, Ramakers IHGB, Rouaud O, Laakso M, Engelborghs S, Popp J, Lleó A, Wallin A, Tsolaki M, Teunissen CE, Vandenberghe R, Freund‑Levi Y, Frölich L, Zetterberg H, Streffer J, Lovestone S, Moonen J, van Harten A, Veverová K, Legdeur N, den Braber A, Damian D, Hall A, Bralten J, Fanelli G, Franke B, Poelmans G, Bulló M, Jimenez‑Murcia S, Fernandez‑Arande F, Salvadó JS, Dalsgaard S, Visser PJ, Vos SJB. The association of diabetes with Alzheimer’s disease biomarkers and vascular burden across European aging and memory clinic cohorts. Alzheimers Dement. 2025 Oct;21(10):e70804. doi: 10.1002/alz.70804 IF: 11.1 Q1 . PMID: 41165072 IF: 11.1 Q1 ; PMCID: PMC12573102 IF: 11.1 Q1 .
2. Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413–446. doi:10.1016/S0140‑6736(20)30367‑6.
3. Biessels GJ, Despa F. Cognitive decline and dementia in diabetes mellitus: mechanisms and clinical implications. Nat Rev Endocrinol. 2018;14(10):591–604. doi:10.1038/s41574‑018‑0093‑4.