Highlight
- Robotic (Da Vinci-assisted) and conventional laparoscopic Nissen fundoplication yield similar patient-reported outcomes and complication rates in GERD treatment.
- No significant differences in postoperative dysphagia, proton pump inhibitor use, intraoperative complications, or long-term failure between techniques were found.
- Robotic surgery consistently involves longer operative times and incurs substantially higher costs without evident clinical benefits.
- Current evidence challenges the routine adoption of robotic platforms in antireflux surgery pending improvements in cost-effectiveness and efficiency.
Study Background
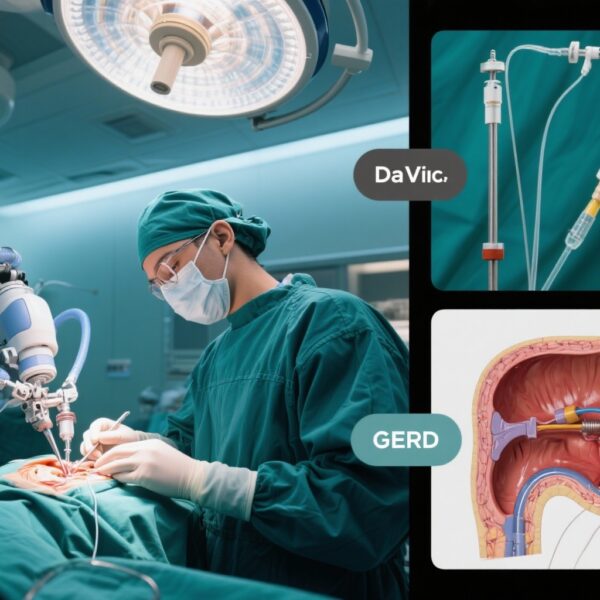
Gastroesophageal reflux disease (GERD) is a prevalent condition characterized by the retrograde flow of gastric contents into the esophagus, causing symptoms such as heartburn, regurgitation, and potential esophageal injury. When medical therapy with proton pump inhibitors (PPIs) fails or when patients prefer surgical management, Nissen fundoplication is a standard surgical intervention aimed at restoring lower esophageal sphincter competence. Conventionally performed via laparoscopy, this procedure has been increasingly adapted to robotic platforms, notably the Da Vinci Surgical System, which offers enhanced dexterity and three-dimensional visualization.
Despite the growing adoption of robotic surgery, its purported clinical benefits over conventional laparoscopy for antireflux surgery remain controversial. Prior meta-analyses produced conflicting results about patient-centered outcomes, operative metrics, and long-term success, with concerns raised about cost and operative time. In this context, a rigorous comparison based solely on randomized controlled trials (RCTs) is essential to delineate the true advantages and limitations of robotic-assisted Nissen fundoplication.
Study Design
This systematic review and meta-analysis by Mirza et al. was prospectively registered with PROSPERO (CRD420251139110) to comprehensively compare Da Vinci-assisted versus conventional laparoscopic Nissen fundoplication. The authors performed an extensive literature search across multiple databases—including MEDLINE, Embase, Cochrane CENTRAL, Web of Science, Scopus, ClinicalTrials.gov, WHO ICTRP, and grey literature—up to August 2025.
Included studies were restricted to RCTs comparing the two techniques in adult patients with GERD undergoing Nissen fundoplication. Primary outcomes of interest were postoperative dysphagia (a critical patient-reported symptom), proton pump inhibitor use post-surgery, and intraoperative complications. Secondary endpoints included reoperation rates, operative time, length of hospital stay, and conversion to open surgery. The meta-analysis applied random-effects models to calculate risk ratios (RR) and mean differences (MD), with evidence quality assessed by the GRADE approach.
Key Findings
The meta-analysis incorporated data from four RCTs, comprising 160 patients: 79 underwent Da Vinci robot-assisted and 81 received conventional laparoscopic Nissen fundoplication.
Primary Outcomes
- Early postoperative dysphagia: Rates were similar between groups (RR 1.05; 95% CI 0.45-2.45), suggesting no difference in patient discomfort related to swallowing dysfunction soon after surgery.
- Postoperative PPI use: No statistically significant difference was observed (RR 0.97; 95% CI 0.25-3.79), indicating comparable reflux control effectiveness.
- Intraoperative complications: Occurred infrequently and did not differ significantly (RR 0.43; 95% CI 0.07-2.81), suggesting equivalent safety profiles.
Secondary Outcomes
- Reoperation rates: No significant differences were found (RR 1.65; 95% CI 0.40-6.90), implying similar long-term procedural success.
- Length of hospital stay: Identical between groups (MD -0.03 days; 95% CI -0.41 to 0.36), reflecting comparable recovery periods.
- Conversion to open surgery rates: Low and similar (RR 1.23; 95% CI 0.19-7.99), indicating similar feasibility and technical difficulty.
- Operative time: Considerable heterogeneity was noted. Sensitivity analysis removing one outlier study revealed significantly longer operative times with robotic surgery (MD 40.28 minutes; p < 0.00001), consistent with prior reports of increased duration related to robotic setup and docking.
Expert Commentary
This carefully performed meta-analysis focusing solely on RCT evidence provides compelling insight into the comparative clinical effectiveness of robotic and laparoscopic Nissen fundoplication. The lack of significant differences in critical patient-centered outcomes such as dysphagia and PPI dependence suggests that the added expense and technical complexity of robotics may not translate into clinical superiority. The consistency of operative times being longer in robotic procedures—once outliers are controlled for—also calls into question workflow efficiency.
The limitations include the relatively small total patient number and limited geographical distribution of trials, warranting cautious extrapolation to broader populations. Furthermore, rapid advancements in robotic technology and surgeon expertise could alter operative times and outcomes in future studies. Cost analysis, although mentioned as a concern, was not directly quantified here but remains a pivotal consideration given the high purchase and maintenance costs of robotic platforms.
Current clinical guidelines, including those from the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), emphasize laparoscopic Nissen fundoplication as a standard approach with established efficacy and safety. Robotic surgery may be reserved for complex cases or centers with specific expertise until more robust evidence of benefit and cost-effectiveness emerges.
Conclusion
This systematic review and meta-analysis of RCTs demonstrate that Da Vinci robotic-assisted Nissen fundoplication offers no significant advantages over conventional laparoscopy in terms of patient-reported outcomes, postoperative complications, or long-term durability in GERD management. Robotic procedures, while safe, involve longer operative times and heightened costs without clear clinical benefits, challenging their routine use. Further research to optimize robotic efficiency and cost should precede wider implementation in antireflux surgery.
Funding and Clinical Trials Registration
The study was prospectively registered on PROSPERO (CRD420251139110). No specific funding source was noted in the published meta-analysis.
References
Mirza W, Khan ME, Uneeb M, Khan HM, Dadan S, Awan AR, Nadeem MA, Chatha HN. Da Vinci-assisted vs laparoscopic nissen fundoplication for GERD: a systematic review and meta-analysis of randomized controlled trials on patient-reported outcomes, dysphagia, and long-term failure. J Robot Surg. 2025 Oct 11;19(1):678. doi: 10.1007/s11701-025-02869-2. PMID: 41075046.
Richards WO, et al. Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines on the surgical treatment of GERD. Surg Endosc. 2023;37(5):2340-2352.
Oelschlager BK, Bell RH Jr. Laparoscopic versus robotic surgery in gastrointestinal procedures: current evidence and future directions. Gastroenterol Clin North Am. 2024;53(1):23-42.