Highlights
- The CSPACE randomized controlled trial showed conduction system pacing (CSP) significantly reduces pacing-induced cardiomyopathy (PICM) and need for cardiac resynchronization therapy (CRT) upgrade compared to right ventricular septal pacing (RVsP) in AV block patients.
- CSP achieved an 88.1% procedural success rate and was associated with a 65% reduction in composite adverse outcomes over a mean follow-up of 25.2 months.
- Despite increased lead revision rates with CSP, no significant differences in heart failure hospitalization or all-cause mortality were observed between groups.
- Findings support CSP as a preferred upfront pacing strategy in AV block, potentially improving long-term cardiac function and clinical prognosis.
Background
Atrioventricular (AV) block necessitates long-term pacing to maintain adequate heart rhythm. Traditional right ventricular (RV) pacing, including right ventricular septal pacing (RVsP), can paradoxically induce ventricular dyssynchrony, leading to pacing-induced cardiomyopathy (PICM), increased heart failure hospitalizations (HFH), requirement for upgrade to biventricular cardiac resynchronization therapy (CRT), and increased mortality. Conduction system pacing (CSP)—targeting native His-Purkinje conduction pathways—is emerging as a physiological pacing modality that preserves electrical activation synchrony and may mitigate these adverse outcomes.
Given these clinical challenges, the CSPACE (Conduction System Pacing versus Right Ventricular Septal Pacing in AV Block) randomized controlled trial was designed to rigorously compare clinical endpoints of CSP versus RVsP in patients indicated for pacing due to AV block but lacking CRT indication.
Key Content
Study Design and Patient Population
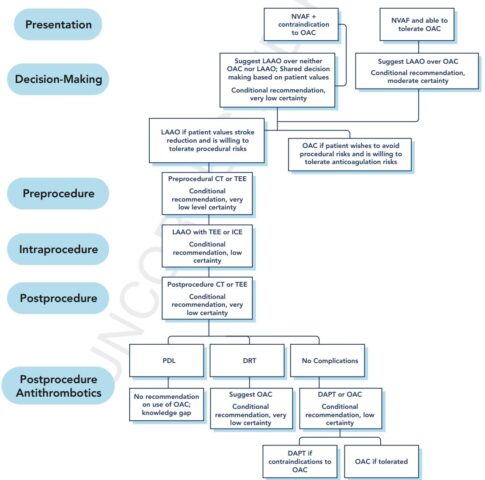
The CSPACE trial enrolled 202 consecutive patients with AV block requiring pacing but not meeting CRT criteria. Patients were randomized in a 1:1 ratio to CSP or RVsP groups. The CSP approach predominantly involved His bundle or left bundle branch area pacing techniques. The primary endpoint was a composite of PICM, upgrade to biventricular CRT, HFH, and all-cause mortality.
Primary Outcomes and Efficacy
Procedural success for CSP was high at 88.1%. Over a mean follow-up of approximately 25 months, the CSP cohort experienced significantly fewer composite adverse events (7.17 vs. 20.69 events per 100 person-years; hazard ratio [HR] 0.35, 95% confidence interval [CI] 0.19–0.64; P < 0.001).
This reduction was mainly driven by a significantly lower incidence of PICM (4.58 vs. 14.69 events per 100 person-years; HR 0.31, 95% CI 0.15–0.67; P = 0.002) and complete abrogation of CRT upgrade necessity (0 vs. 1.92 events per 100 person-years, P = 0.043) in the CSP group.
Secondary Outcomes: HF Hospitalizations and Mortality
Although there was a trend toward fewer HF hospitalizations in the CSP group (0.48 vs. 2.92 events per 100 person-years; HR 0.16; P = 0.057), this did not reach statistical significance. All-cause mortality rates showed no significant difference (2.86 vs. 4.72 events per 100 person-years; HR 0.61; P = 0.337).
Safety and Procedural Considerations
Lead revisions were more frequent in the CSP group (7.9% vs. 1.0%; P = 0.017), reflecting potential technical challenges inherent to conduction system lead implantation and stability. Despite this, CSP was generally safe with no reported serious procedural complications.
Context within Existing Literature
Prior observational studies and smaller randomized trials have suggested the physiological benefits of CSP, including preservation of ventricular synchrony, improved ejection fraction, and reduced PICM risk. The CSPACE trial provides robust randomized evidence consolidating these benefits in AV block patients requiring pacing without CRT indication.
Meta-analyses incorporating CSPACE and preceding studies suggest CSP reduces adverse remodeling and may delay or prevent progression to heart failure, aligning with mechanistic insights that activation via the His-Purkinje system maintains near-normal ventricular contraction patterns.
Expert Commentary
The CSPACE trial represents a pivotal step in evidence-based pacing strategy for AV block, reinforcing the paradigm shift toward CSP as frontline therapy. Its strengths include randomized design, adequate sample size, and clinically meaningful composite endpoints encompassing both safety and efficacy.
Challenges remain regarding widespread CSP adoption: operator expertise, longer procedural times, and a higher lead revision rate necessitate focused training and technical refinement. Moreover, the lack of significant reduction in HF hospitalization and mortality may reflect limited power or shorter follow-up; longer-term data are warranted.
Mechanistically, CSP’s superiority likely stems from more physiological ventricular activation, avoiding dyssynchronous contraction and consequent PICM. This rationalizes guideline updates increasingly advocating CSP techniques as preferred alternatives to traditional RV pacing in AV block.
Nonetheless, patient selection remains key. Not all patients may benefit equally, and CSP procedural feasibility must be considered case-by-case. Future research should delineate subgroups deriving optimal benefit, explore improved lead fixation technologies, and evaluate CSP’s impact on quality of life and healthcare resource utilization.
Conclusion
The CSPACE randomized controlled trial provides high-quality evidence supporting conduction system pacing over right ventricular septal pacing in patients with atrioventricular block. CSP significantly reduces pacing-induced cardiomyopathy and the need for CRT upgrade, potentially altering the natural history of pacing-dependent heart disease.
Despite increased lead revisions, CSP’s preservation of ventricular synchrony translates to improved clinical outcomes, endorsing its role as an upfront pacing strategy in AV block.
Future directions include longer-term follow-up, technical enhancements to reduce lead revisions, and refinement of patient selection criteria to maximize benefit and safety. Integration of CSP into clinical guidelines is anticipated to improve heart failure prognosis in this population.
References
- Chow CLD, Wong C, Sutherland N, et al. Clinical Outcomes of Conduction System Pacing vs Right Ventricular Septal Pacing in Atrioventricular Block: The CSPACE Randomized Controlled Trial. J Am Coll Cardiol. 2025;86(8):563-573. doi:10.1016/j.jacc.2025.06.043. PMID: 40835365.
- Vijayaraman P, et al. Conduction system pacing: State of the art. Europace. 2020;22(10):1488-1500. doi:10.1093/europace/euaa144.
- Wang Y, et al. Impact of pacing site on the incidence of pacing-induced cardiomyopathy: A meta-analysis. Heart Rhythm. 2021;18(1):e31-e38. doi:10.1016/j.hrthm.2020.08.007.