Background and Disease Burden
Primary sclerosing cholangitis (PSC) is a chronic, progressive cholangiopathy characterized by inflammation and fibrosis of the bile ducts, ultimately leading to cholestasis, cirrhosis, and increased risk of hepatobiliary malignancies. Despite significant morbidity and the potential need for liver transplantation, the pathogenesis of PSC remains incompletely understood, and current therapeutic options are limited. The identification of novel mediators involved in PSC pathophysiology is critical for developing targeted therapies.
Study Design and Methods
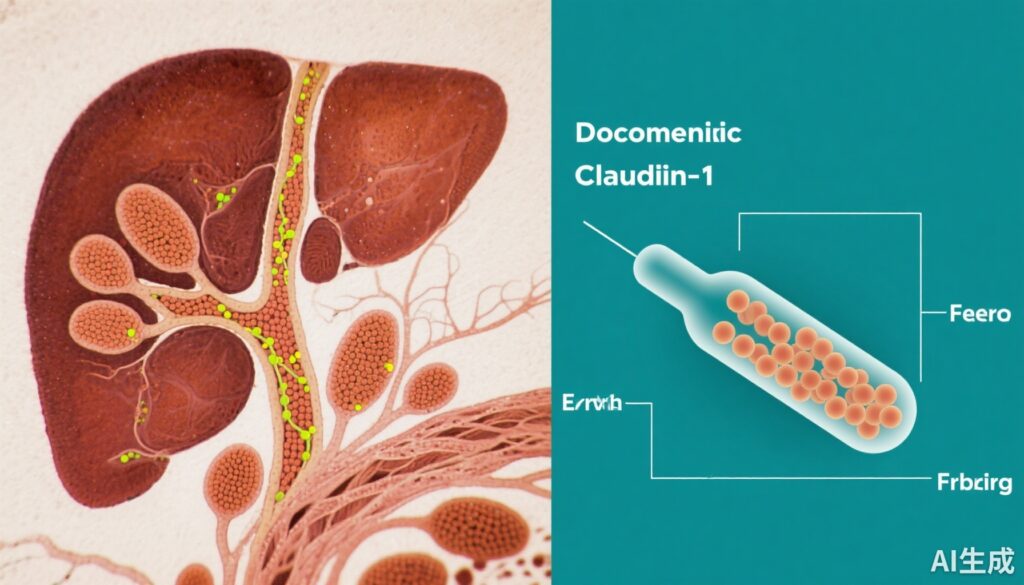
This study investigated the role of Claudin-1 (CLDN1), a transmembrane tight junction protein integral to liver epithelial cell communication, in the pathogenesis and treatment of PSC. Five independent PSC patient cohorts provided liver tissue samples analyzed using advanced single-cell RNA sequencing (scRNAseq), spatial transcriptomics, and multiplex proteomics to characterize CLDN1 expression patterns and associated cell phenotypes.
Functional studies comprised both genetic and immunological interventions. Conditional liver epithelial-specific CLDN1 knockout mouse models of PSC and cholangiopathies were established to study loss-of-function effects. In parallel, therapeutic administration of CLDN1-specific monoclonal antibodies (mAbs) was evaluated for their efficacy in ameliorating liver injury and fibrosis. Human cell-based models supplemented by perturbation assays provided mechanistic insights into the signaling pathways and cellular responses influenced by CLDN1.
Key Findings
CLDN1 Upregulation in PSC: Analysis revealed a marked upregulation of CLDN1 in PSC patient livers, particularly in diseased cholangiocytes and cholestatic periportal hepatocytes. Spatial transcriptomics demonstrated elevated CLDN1 expression correlating with the advancement of disease severity and progression. This upregulation was concomitant with the activation of pro-inflammatory and profibrotic pathways, including heightened signals associated with fibrosis and immune cell recruitment.
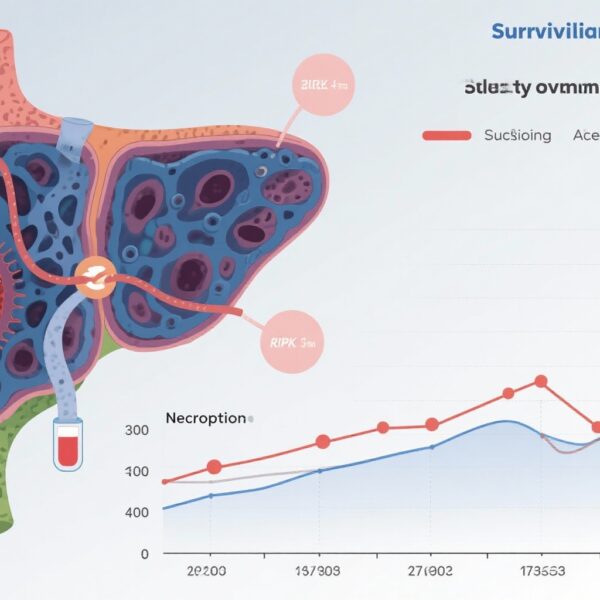
Therapeutic Impact of CLDN1 Blockade: In murine PSC models, both genetic ablation of CLDN1 in liver epithelial cells and administration of CLDN1-specific mAbs significantly improved liver function. Improvements were evidenced by reductions in hepatic fibrosis, cholestasis, and markers of liver injury. The intervention also attenuated the ductular reaction, a hallmark of biliary injury and fibrogenesis.
Mechanistic Insights: Monoclonal antibody treatment modulated signaling cascades within cholangiocytes and hepatocytes, suppressing pro-inflammatory and profibrotic gene expression programs. This mechanistic inhibition likely underlies the observed therapeutic effects, suggesting that CLDN1 acts as a critical mediator of pathologic cell-cell communication driving PSC progression.
Expert Commentary
The identification of CLDN1 as a key intestinal junction protein implicated in PSC pathogenesis provides a compelling molecular target for intervention. Current therapies for PSC are limited and largely supportive, underscoring the need for disease-modifying treatments. This study’s use of cutting-edge spatial and single-cell technologies in concert with clinically relevant animal models adds robustness to the data supporting CLDN1’s pathogenic role.
However, translation to clinical practice requires thorough safety evaluation, as tight junction proteins like CLDN1 play essential roles in maintaining epithelial integrity across organs. The specificity of monoclonal antibodies and their functional impact need careful elucidation in human trials. Additionally, heterogeneity in PSC patient populations and the influence of associated inflammatory bowel disease should be considered when designing such clinical studies.
Conclusion
This multidisciplinary preclinical investigation delineates a novel pathogenic mechanism implicating Claudin-1 in PSC and presents CLDN1-specific monoclonal antibodies as a promising therapeutic candidate. The correlation between CLDN1 expression and disease progression in patients, combined with therapeutic efficacy in animal models, strongly supports further clinical development.
Targeting CLDN1 may overcome the current therapeutic void in PSC, potentially reducing fibrosis and cholestasis and improving patient outcomes. Future clinical trials will be essential to validate safety and efficacy, and to establish CLDN1 blockade as a disease-modifying therapy in PSC.
Funding and Disclosures
The study was supported by multiple international consortia specializing in hepatology and liver disease research. Potential conflicts of interest, detailed methodology, and data accessibility can be referenced in the original publication.
References
Del Zompo F, Crouchet E, Ostyn T, et al. Claudin-1 is a mediator and therapeutic target in primary sclerosing cholangitis. J Hepatol. 2025 Aug 20:S0168-8278(25)02440-7. doi: 10.1016/j.jhep.2025.08.005. Epub ahead of print. PMID: 40846184.