Introduction: The Cancer Conundrum in Humans and Our Primate Relatives
Cancer remains one of the leading health threats to humans worldwide, with over ten million new cases annually and high mortality rates despite advances in medical care. Yet, an intriguing biological puzzle exists: humans appear to suffer from cancer much more frequently than their closest evolutionary relatives, such as chimpanzees. This observation has sparked a scientific quest to uncover why the human immune system might be less effective at combating tumors compared to that of other primates.
Recently, a groundbreaking study from the University of California, Davis Comprehensive Cancer Center has identified a critical molecular difference involving a protein called plasmin (also known as fibrinolysin) that helps to explain these disparities. This discovery not only advances our understanding of evolutionary biology but also opens new avenues for improving cancer immunotherapy, especially for patients with solid tumors who have limited treatment options.
The Immune System: Our Innate Cancer Fighter
Every day, our bodies generate countless abnormal cells that have the potential to transform into cancer if left unchecked. Fortunately, the immune system acts as a vigilant guardian, with specialized cells known as T lymphocytes patrolling our tissues to recognize and eliminate these rogue cells before they can become malignant. Among these, cytotoxic T cells are crucial players; they kill cancer cells by releasing lethal molecules that induce cell death.
In theory, this immune surveillance should effectively prevent cancer development. However, in reality, many tumors manage to evade immune destruction and progress. Understanding how tumors escape immune control has been a central focus of cancer research.
The Evolutionary “Flaw”: Plasmin’s Double-Edged Role
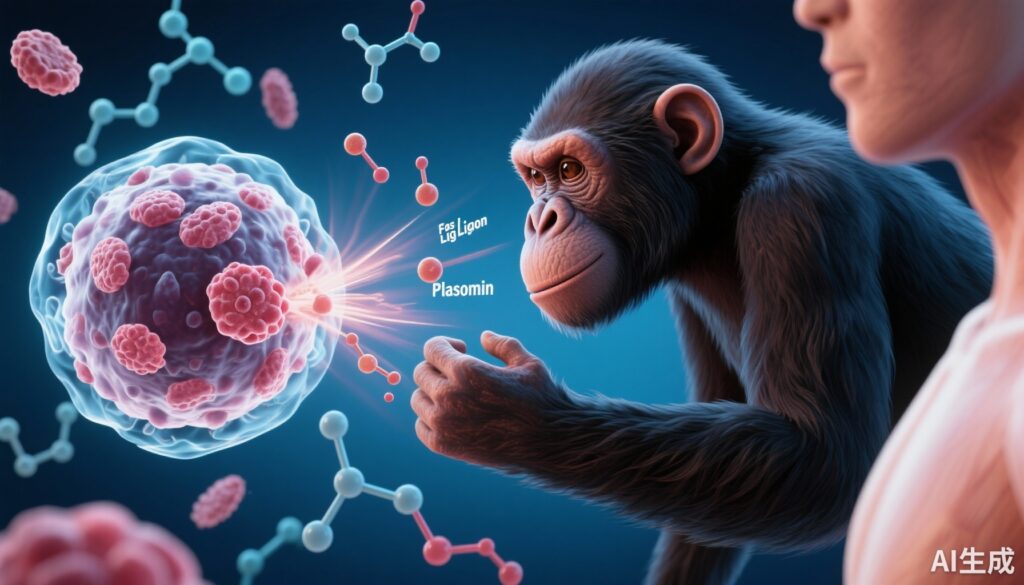
The UC Davis team uncovered that plasmin, a protein best known for its role in dissolving blood clots and maintaining normal blood flow, has an unexpected and detrimental impact on the immune attack against cancer. Plasmin chemically cleaves and disrupts Fas ligand (FasL), a death-inducing molecule expressed on cytotoxic T cells responsible for killing tumor cells.
In humans, although T cells produce FasL to trigger cancer cell apoptosis, plasmin rapidly cuts and inactivates this molecule before it reaches its target. This biochemical interference effectively disarms one of the immune system’s primary weapons against tumors, compromising the ability of T cells to eliminate cancer.
By contrast, chimpanzees possess a slightly different version of FasL that is resistant to plasmin cleavage. This evolutionary divergence means that chimpanzee T cells retain full killing potency, contributing to their remarkably lower cancer incidence.
This discovery reveals an evolutionary trade-off wherein humans, possibly due to changes in the immune system or coagulation pathways, lost some anti-cancer efficacy, leaving them more vulnerable to tumor development.
Strategies to Restore T Cell Potency: Targeting Plasmin to Enhance Immunotherapy
Recognizing that plasmin-mediated cleavage of FasL is a key barrier to effective anti-tumor immunity, researchers have explored therapeutic approaches to “protect” FasL and restore T cell cytotoxicity. Two main strategies have shown promise in preclinical studies:
1. Plasmin Inhibitors: These drugs block plasmin activity, preventing it from cutting FasL, thus preserving T cell killing function.
2. Protective Antibodies: Engineered antibodies selectively bind to FasL, shielding it from plasmin degradation without interfering with immune cell activity.
Animal experiments demonstrated that either approach significantly boosts immune cell-mediated tumor killing, leading to better control of solid cancers. When combined with existing immunotherapies, such as checkpoint inhibitors, these strategies have the potential to improve treatment outcomes by overcoming current immune resistance mechanisms.
Challenges and Cautions: Not a Magic Bullet Yet
Despite these exciting findings, several hurdles remain before such treatments can be widely applied in humans.
– Safety and Side Effects: Plasmin plays a vital role in preventing blood clots and maintaining cardiovascular health. Inhibiting plasmin excessively could increase the risk of unwanted thrombosis or bleeding complications.
– Complexity of Cancer: Cancer is a multifaceted disease involving numerous pathways. Targeting a single mechanism may not suffice; combinatory approaches may be necessary.
– Clinical Validation: These findings are preliminary and require extensive testing in diverse animal models and clinical trials to confirm efficacy and safety in patients.
Nevertheless, this research marks a pivotal step towards personalized cancer immunotherapy tailored to tumor biology and individual immune profiles.
Expert Insight
Dr. Jean Legembre, the lead investigator of the study, emphasizes: “While overcoming plasmin’s interference is not a cure-all, it represents a crucial advancement in enhancing the immune system’s natural arsenal against difficult-to-treat solid tumors. Our work lays the foundation for next-generation immunotherapies that could improve survival and quality of life for many patients.”
Patient Scenario: Sarah’s Journey Towards New Therapeutic Hope
Consider Sarah, a 52-year-old woman diagnosed with an aggressive form of solid tumor. After several rounds of standard therapies, her cancer showed resistance, and her oncologist suggested participation in a clinical trial involving immunotherapy combined with a novel plasmin inhibitor. By blocking plasmin-mediated FasL cleavage, Sarah’s immune system regained its capacity to attack tumor cells more effectively.
Over the next months, her tumor shrank significantly, demonstrating the potential of this innovative approach. While this is just one example, it illustrates how insights from evolutionary biology and molecular immunology can translate into transformative patient care.
Conclusion: Evolutionary Biology Illuminates New Paths in Cancer Treatment
The higher incidence of cancer in humans compared to chimpanzees is partly explained by an evolutionary vulnerability: human Fas ligand is susceptible to cleavage by plasmin, weakening immune cell-mediated cancer cell killing.
This newly uncovered mechanism offers a promising target to enhance immunotherapy for challenging solid tumors. Although more research is required to translate these findings into safe and effective clinical treatments, the study from the University of California, Davis stands as a testament to the power of combining evolutionary insights with cutting-edge biomedical science.
By understanding and overcoming the evolutionary “flaws” in our immune system, we move closer to developing more effective personalized therapies, ultimately improving cancer outcomes worldwide.
References
Wamba BEN, Mondal T, Freenor VF, Shaheed M, Pang O, Bedinger D, Legembre P, Devel L, Bhatnagar S, Leiserowitz GS, Tushir-Singh J. Evolutionary regulation of human Fas ligand (CD95L) by plasmin in solid cancer immunotherapy. Nat Commun. 2025 Jul 1;16(1):5748. doi: 10.1038/s41467-025-60990-0. PMID: 40593750; PMCID: PMC12217004.