Highlight
– The BHF PROTECT-TAVI trial evaluated the effect of cerebral embolic protection (CEP) on neurocognitive outcomes after TAVI in 3535 patients.
– No significant difference was found between CEP and control groups in cognitive performance measured by the telephone Montreal Cognitive Assessment at 6–8 weeks.
– Incidence of significant cognitive decline (≥3-point t-MoCA drop) was similar between groups.
– Findings were consistent across all examined subgroups and robust in sensitivity analyses, questioning the cognitive protective value of CEP devices in TAVI.
Study Background and Disease Burden
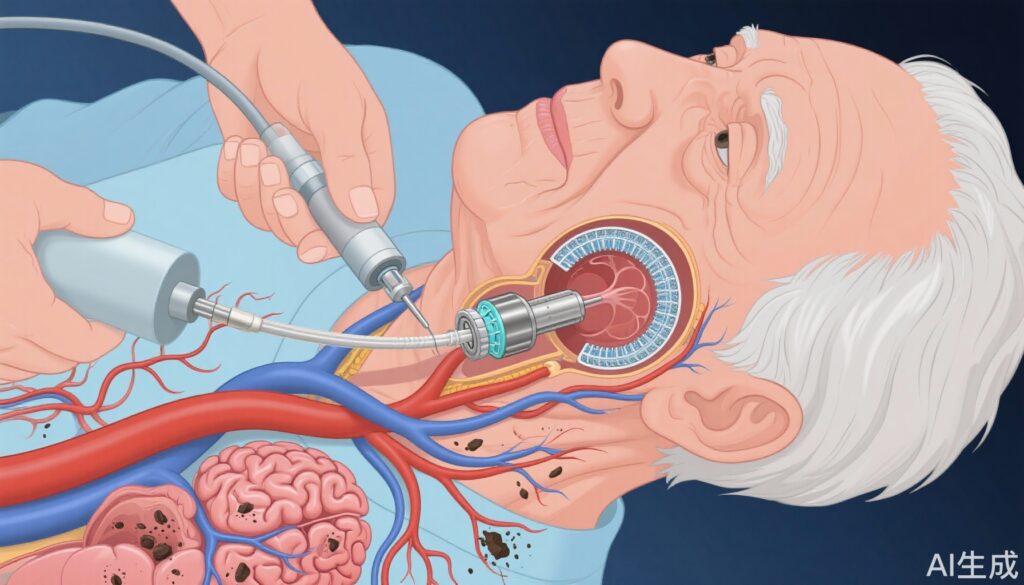
Transcatheter aortic valve implantation (TAVI) has become a widely used minimally invasive procedure for patients with severe aortic stenosis, particularly in elderly populations high-risk for surgery. While TAVI reduces mortality and improves symptomatic status, it carries a risk of neurologic complications including clinically overt stroke and subtle neurocognitive decline. This cognitive impairment after TAVI is increasingly recognized as an important determinant of quality of life and longer-term functional status.
Neurocognitive decline after TAVI is thought to be largely related to cerebral embolization of procedural debris such as valve tissue or calcium fragments. These emboli can cause microvascular ischemic injury and brain infarcts, even in the absence of clinical stroke symptoms. Consequently, cerebral embolic protection (CEP) devices, such as the SENTINEL system (Boston Scientific), have been developed to capture and remove embolic material during TAVI procedures, aiming to reduce stroke risk and preserve neurocognitive function.
Despite their theoretical benefit, the clinical impact of CEP devices on cognitive outcomes remains uncertain. Prior studies have focused predominantly on clinical stroke rates, with inconsistent evidence on cognitive preservation. Therefore, robust data from large randomized trials assessing cognitive function are essential to establish the role of CEP in TAVI.
Study Design
This article reports a secondary analysis from the British Heart Foundation (BHF) PROTECT-TAVI randomized controlled trial, conducted at 33 centers across the United Kingdom. The trial enrolled 3535 patients with severe aortic stenosis, randomized in a 1:1 ratio to TAVI with the SENTINEL cerebral embolic protection device (Sentinel CEP group) or TAVI alone (Control group).
The current analysis focuses on those patients who underwent cognitive assessments. The primary outcome was the mean change in the telephone version of the Montreal Cognitive Assessment (t-MoCA) score from baseline to 6–8 weeks post-TAVI. The t-MoCA is a validated screening tool for mild cognitive impairment suitable for telephone administration.
The secondary outcome was the proportion of patients experiencing a clinically meaningful cognitive decline defined as a ≥3-point drop in t-MoCA score between baseline and follow-up. Analyses were adjusted for baseline cognitive performance and assessed for consistency across predefined subgroups.
Key Findings
The cognitive analysis included 3535 patients (mean age 81.0 years, 37.7% female), with 1763 assigned to CEP and 1772 to control. At baseline, the median t-MoCA score was 18 (IQR 16 to 20), indicating mild cognitive impairment common in this elderly population.
At 6–8 weeks post-TAVI, the median t-MoCA improved modestly to 20 (IQR 17 to 21) across all patients, reflecting potential benefits from symptom relief and restoration of cardiac function.
Adjusted mean changes in t-MoCA scores from baseline to follow-up were 0.83 (95% CI 0.70 to 0.96) in the CEP group and 0.91 (95% CI 0.79 to 1.04) in the control group. The between-group difference was not statistically significant (−0.07; 95% CI −0.22 to 0.09; p=0.42).
Regarding clinically significant cognitive decline, 8.7% (154/1763) of the CEP group experienced a ≥3-point drop in t-MoCA versus 8.0% (142/1772) in controls (risk difference 0.72%; 95% CI −1.10 to 2.55%; p=0.44), a non-significant difference.
Results were consistent after sensitivity analyses and showed no significant interaction across demographic or clinical subgroups including differences by age, sex, baseline cognitive status, or procedural factors.
Overall, the data strongly suggest that placement of a cerebral embolic protection device during TAVI does not confer a measurable benefit on neurocognitive outcomes at medium-term follow-up.
Expert Commentary
These findings challenge the assumption that filtering of procedural emboli leads to cognitive preservation after TAVI. While prior smaller studies hinted at reduced brain lesion volume or lower clinical stroke rates with CEP, the lack of cognitive benefit observed here raises important questions.
One explanation could be that microemboli escaping CEP filters or distal embolization beyond protection zones still cause brain injury. Additionally, cognitive impairment post-TAVI is multifactorial, involving not only embolic events but also hemodynamic changes, inflammation, and pre-existing cerebrovascular disease.
Furthermore, the t-MoCA, although validated and feasible for large trials, may lack sensitivity for subtle cognitive changes. The follow-up period of 6–8 weeks might not capture late cognitive effects or recovery trajectories.
From a clinical perspective, these results suggest that routine use of CEP devices solely to preserve cognition may not be justified. However, ongoing research with more sensitive neuroimaging, longer follow-up, and exploration of patient subgroups is needed.
The BHF PROTECT-TAVI trial thus informs guideline committees and practitioners about the real-world neurocognitive impact of CEP and emphasizes the importance of comprehensive risk-benefit assessment before adoption.
Conclusion
In summary, the secondary analysis of the large, pragmatic BHF PROTECT-TAVI randomized trial demonstrates no significant cognitive benefit from cerebral embolic protection devices used during transcatheter aortic valve implantation. Despite the theoretical reduction in cerebral embolic load, no differences were observed in cognitive function measured by telephone Montreal Cognitive Assessment at 6–8 weeks or in clinically meaningful cognitive declines.
Clinicians should carefully consider these findings when weighing the routine use of CEP during TAVI. Further investigations are warranted to elucidate mechanisms of neurocognitive impairment post-TAVI and to identify patient populations that might benefit from cerebral protection strategies or alternative interventions.
References
Kennedy J, Blackman DJ, Dodd M, Poggesi A, Read L, Jamal Z, Evans R, Clayton T, Kharbanda RK, Hildick-Smith D; BHF PROTECT-TAVI Investigators. Impact of Cerebral Embolic Protection On Cognitive Function Following Transcatheter Aortic Valve Implantation: Data From the BHF PROTECT-TAVI Randomized Trial. Circulation. 2025 Aug 30. doi: 10.1161/CIRCULATIONAHA.125.076761. Epub ahead of print. PMID: 40884786.