Highlight
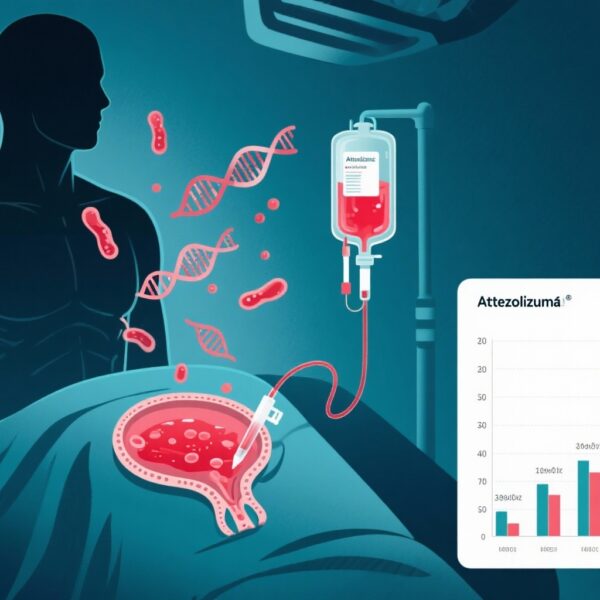
– The phase 3 IMvoke010 trial investigated atezolizumab as maintenance therapy in high-risk locally advanced squamous cell carcinoma of the head and neck (LA SCCHN) after definitive multimodal treatment.
– Atezolizumab did not significantly improve event-free survival or overall survival compared with placebo after a median follow-up of approximately 3.9 years.
– The safety profile of atezolizumab was consistent with expectations; no new safety signals emerged.
– These results underline the continued unmet need for effective adjuvant therapies in LA SCCHN and question the role of checkpoint inhibitors in this patient population.
Study Background
Locally advanced squamous cell carcinoma of the head and neck (LA SCCHN) is a heterogeneous malignancy arising from sites such as the oral cavity, larynx, hypopharynx, and oropharynx. Management typically involves multimodal definitive treatment, including surgery, radiation therapy, and chemotherapy. Despite aggressive therapy, patients with high-risk disease—characterized by advanced tumor stage or adverse pathological features—face suboptimal outcomes, including high rates of local recurrence and distant metastases.
Immune checkpoint inhibitors targeting the programmed death-ligand 1 (PD-L1)/programmed death-1 (PD-1) axis have revolutionized treatment paradigms in recurrent or metastatic head and neck cancer, but their efficacy in the maintenance/adjuvant setting remains unclear. The IMvoke010 study was designed to address this pressing clinical question by evaluating atezolizumab, an anti-PD-L1 monoclonal antibody, as maintenance therapy after definitive treatment in patients at high risk of progression.
Study Design and Methods
IMvoke010 was a global, phase 3, randomized, double-blind, placebo-controlled clinical trial conducted at 128 sites across 23 countries from April 2018 to February 2020.
Eligibility criteria included adults with stage IVa or IVb LA SCCHN (oral cavity, larynx, hypopharynx, or HPV-negative oropharynx) or stage III HPV-positive oropharynx cancer, who had completed definitive multimodal treatment without evidence of disease progression. Patients were randomized 1:1 to receive atezolizumab 1200 mg or placebo intravenously every three weeks for up to one year or until disease recurrence, progression, unacceptable toxicity, or withdrawal of consent.
The primary endpoint was investigator-assessed event-free survival (EFS), defined as the time from randomization to local/regional recurrence, distant metastases, new primary tumor, or death from any cause. Key secondary endpoints included overall survival (OS) and safety.
Key Findings
A total of 406 patients were randomized, with balanced baseline demographics between atezolizumab (n=203) and placebo (n=203) arms. The median age was approximately 60 years, predominantly male, and racially diverse.
After a median follow-up of 46.5 months (nearly 4 years), median event-free survival was 59.5 months (95% CI, 46.8 to not estimable) with atezolizumab versus 52.7 months (95% CI, 41.4 to not estimable) with placebo. The hazard ratio for event or death was 0.94 (95% CI, 0.70–1.26; P=0.68), indicating no statistically significant benefit.
Similarly, overall survival at 24 months was comparable: 82.0% in the atezolizumab arm versus 79.2% in the placebo arm, without a statistically significant difference.
Regarding safety, atezolizumab’s profile was consistent with previous reports in head and neck cancer, with no new or unexpected adverse events identified. The incidence of immune-related adverse events was manageable and aligned with known toxicities of checkpoint blockade.
Expert Commentary
The negative results of IMvoke010 highlight the complexity of using immunotherapy as maintenance treatment in LA SCCHN. Unlike the metastatic or recurrent setting, where checkpoint inhibitors have demonstrated survival benefits, the adjuvant setting presents distinct biological and clinical challenges, such as tumor microenvironment differences and heterogeneity of residual disease.
These findings align with recent data from other trials investigating immune checkpoint inhibitors as adjuvant or maintenance therapies in high-risk cancers that have delivered mixed outcomes. Potential explanations include an insufficient immunogenic stimulus in minimal residual disease, immune suppression from prior therapies, or the need for combinational immunomodulatory approaches.
Limitations of the study include the composite endpoint of EFS by investigator assessment, which may introduce variability, as well as challenges in patient selection criteria to identify those most likely to benefit. Further translational research evaluating biomarkers predictive of immunotherapy response in LA SCCHN is warranted.
Conclusions
The IMvoke010 phase 3 trial demonstrated that maintenance therapy with atezolizumab after definitive multimodal treatment did not improve event-free or overall survival in a global population of patients with high-risk locally advanced squamous cell carcinoma of the head and neck. This underscores the ongoing unmet clinical need for novel adjuvant therapeutic strategies in this setting.
Checkpoint inhibition, although a breakthrough in recurrent/metastatic head and neck cancer, has limited efficacy as a postoperative maintenance strategy. Future research should focus on better patient stratification, integration of immune-based biomarkers, and combinational approaches to enhance the therapeutic benefit of immunotherapy in earlier stage disease.
Funding and Trial Registration
IMvoke010 was funded by Genentech, Inc., the developer of atezolizumab. The trial is registered on ClinicalTrials.gov under the identifier NCT03452137.
Reference
Haddad R, Fayette J, Teixeira M, Prabhash K, Mesia R, Kawecki A, Dechaphunkul A, Dinis J, Guo Y, Masuda M, Hsieh CY, Ghi MG, Vaz de Melo Sette C, Harrington K, Tahara M, Saba NF, Lau A, Jiang T, Yan Y, Ballinger M, Kaul M, Matheny C, Cuchelkar V, Wong DJ. Atezolizumab in High-Risk Locally Advanced Squamous Cell Carcinoma of the Head and Neck: A Randomized Clinical Trial. JAMA. 2025 May 13;333(18):1599-1607. doi: 10.1001/jama.2025.1483. PMID: 40079944; PMCID: PMC11907359.