Highlight
- Individuals below 50 years undergoing polypectomy have a comparable risk of metachronous high-risk neoplasia as those 50 years and older when the colonoscopy is performed for screening.
- Risk of recurrent advanced neoplasia peaks around three years post-polypectomy in both age groups.
- The study supports applying current surveillance guidelines, traditionally designed for older adults, to younger populations post-polypectomy.
Study Background and Disease Burden
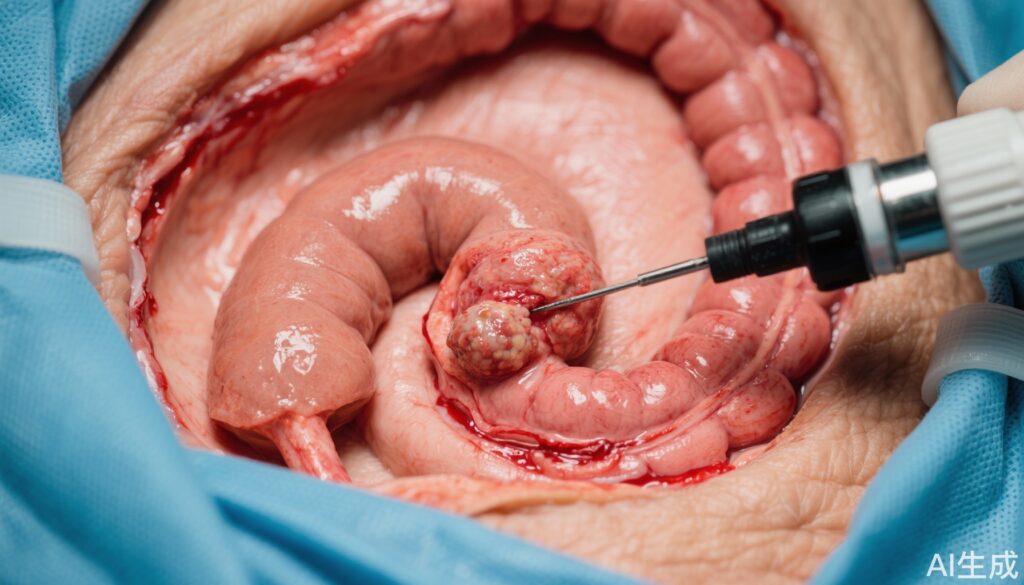
Colorectal cancer (CRC) remains a leading cause of cancer-related morbidity and mortality worldwide. Polypectomy during colonoscopy significantly reduces CRC risk by removing precancerous adenomas and serrated polyps (SPs), recognized precursor lesions. Current colonoscopy surveillance guidelines are predominantly based on evidence derived from populations aged 50 years and older, the traditional screening threshold age due to higher CRC incidence. However, CRC incidence among adults younger than 50 years is increasing globally, posing a challenge given limited data on post-polypectomy surveillance in this younger demographic. There is a clinical imperative to understand whether younger patients, following polypectomy, share similar recurrence risks for high-risk neoplasia to optimize surveillance intervals and improve outcomes.
Study Design
This prospective cohort study analyzed data from the Mass General Brigham Colonoscopy Cohort collected between 2007 and 2023. Participants included adults who underwent at least one follow-up colonoscopy after an index colonoscopy with or without polypectomy. The cohort was stratified by age: individuals younger than 50 years and those 50 years or older. Index colonoscopy findings were categorized into three groups: no polyps, adenomas, and serrated polyps (SPs), including those with synchronous adenomas and SPs. High-risk neoplasia encompassed high-risk adenomas, high-risk serrated polyps, and incident colorectal cancer. The primary outcome was the risk of metachronous (subsequent) high-risk neoplasia assessed via multivariable-adjusted Cox proportional hazards models to estimate hazard ratios (HRs) and 95% confidence intervals (CIs).
Key Findings
A total of 79,694 adults were included: 37,576 without polyps, 26,693 with adenomas, and 15,425 with serrated polyps (including 8,303 with synchronous lesions). Among these, 10,977 (29.2%), 3,385 (12.7%), and 2,659 (17.2%) were under 50 years at diagnosis, respectively.
Across the entire cohort, associations between index polyp findings and subsequent high-risk neoplasia were stronger among younger adults ( 0.05).
Among individuals who underwent screening colonoscopy, the risk for metachronous high-risk neoplasia was markedly elevated for those with index high-risk lesions in both age groups. The relative risk peaked approximately 3 years post-polypectomy, with HRs of 4.60 (95% CI: 3.63 to 5.84) for young adults with high-risk adenomas and 5.59 (95% CI: 3.89 to 8.03) for those with high-risk serrated polyps.
Importantly, no statistically significant difference was identified between age groups regarding the magnitude of risk, implying that the biological behavior and recurrence risk of high-risk neoplasia post-polypectomy are similar regardless of whether patients are below or above age 50.
Expert Commentary
This comprehensive study addresses a critical evidence gap in colorectal cancer surveillance, particularly in young adults who historically have not been the focus of screening guidelines. The rigorous longitudinal design and robust statistical adjustments strengthen the validity of these findings.
The findings imply that metachronous neoplasia biology and recurrence kinetics may be independent of chronological age once initial polyp histopathology and risk features are accounted for. This observation challenges current surveillance paradigms that discontinue or delay surveillance colonoscopy in younger adults post-polypectomy due to perceived lower risk.
However, limitations include potential referral or surveillance bias inherent in a single health system cohort and the relatively shorter average follow-up for younger adults due to later inclusion in routine screening. Future studies in diverse populations and longer-term outcomes will be valuable to confirm these findings.
Current guidelines, such as those from the US Multi-Society Task Force on CRC, might consider revising recommendations to explicitly incorporate younger patients with high-risk lesions detected at screening.
Conclusion
In summary, this prospective evaluation from a large colonoscopy cohort demonstrates that adults younger than 50 years undergoing polypectomy as part of screening face similar risks of developing metachronous high-risk neoplasia as their older counterparts. Risk peaks around three years post-polypectomy, consistent with older populations. These findings support extending current surveillance colonoscopy guidelines, originally based on older adults, to younger patients who undergo polypectomy for high-risk colorectal polyps. As younger onset colorectal cancer incidence rises, clarity on surveillance strategies is essential to optimize early detection and prevention efforts.
References
Chen Y, Padilla Aponte J, Wang K, Du M, Lu Y, Polychronidis G, Song M. Comparative risk of high-risk neoplasia after polypectomy among individuals aged below 50 years versus 50 years and older. Gut. 2025 Aug 24:gutjnl-2025-335275. doi: 10.1136/gutjnl-2025-335275. Epub ahead of print. PMID: 40850745.
American Cancer Society. Colorectal Cancer Facts & Figures 2020-2022. https://www.cancer.org/
US Multi-Society Task Force on Colorectal Cancer. Recommendations for surveillance after polypectomy. Gastroenterology. 2020;158(4):1131-1143.
Rex DK, et al. Serrated colorectal polyps and cancer: new clinical insights. Gastroenterology. 2017;153(3):665-681.