Highlight
– The PRACTICE trial is the first randomized controlled study assessing the safety of leaving rectosigmoid polyps ≤5 mm in situ using AI-assisted optical diagnosis.
– The adenoma detection rate (ADR) was not reduced by leaving non-neoplastic polyps in place, meeting non-inferiority criteria compared with systematic polypectomy.
– No colonoscopy-related complications were observed in either group, highlighting the safety of AI-guided optical diagnosis.
– This approach may reduce unnecessary polypectomies, procedural risks, and healthcare costs while maintaining oncological safety.
Study Background and Disease Burden
Colorectal cancer (CRC) remains a leading cause of cancer-related morbidity and mortality worldwide. Colonoscopy with polypectomy is the cornerstone of CRC screening and prevention by enabling detection and removal of precancerous lesions, primarily adenomas. Current clinical guidelines recommend resection of most polyps; however, for diminutive rectosigmoid polyps (≤5 mm), some guidelines suggest that endoscopists can leave lesions in situ if confidently assessed as non-neoplastic through optical diagnosis. This selective approach aims to avoid unnecessary polypectomies, reducing procedure time, costs, and risk of complications such as bleeding or perforation.
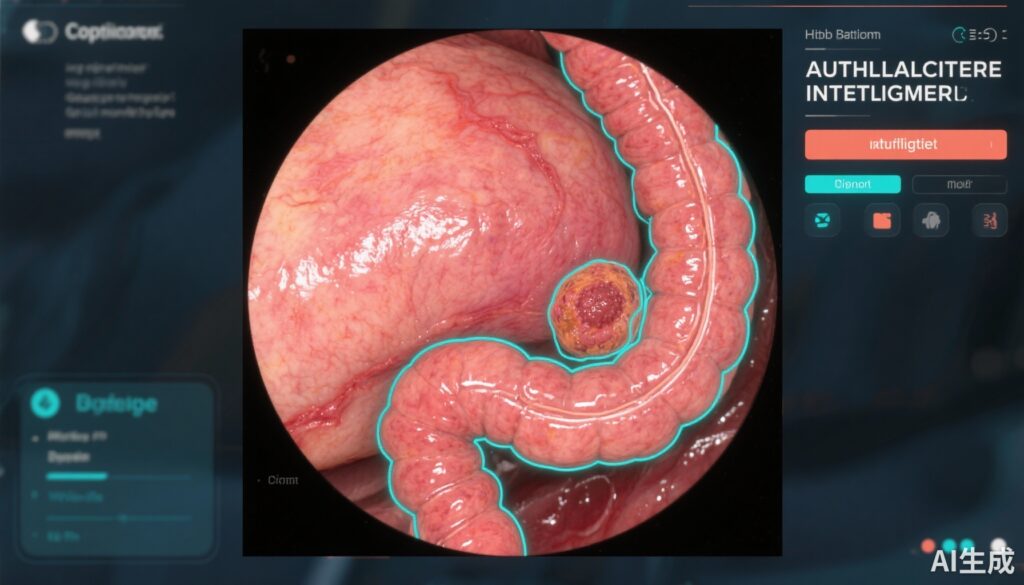
Despite these recommendations, the safety and efficacy of a leave-in-situ strategy guided by optical diagnosis have not been evaluated in randomized controlled trials. Implementation in routine clinical practice is hindered by variable diagnostic accuracy of optical assessment and concerns about missing neoplastic lesions. The advent of artificial intelligence (AI)-assisted computer-aided detection and diagnosis (CADe/CADx) tools has enhanced lesion characterization sensitivity and specificity, providing an opportunity to rigorously evaluate this approach.
Study Design
The PRACTICE study was an open-label, multicentre, randomized controlled trial conducted across four Italian centres, enrolling adults aged 18 years or older undergoing colonoscopy for screening, surveillance, or clinical indications. Patients were randomly assigned 1:1 to either the leave-in-situ group, where endoscopists used AI-assisted optical diagnosis to leave non-neoplastic polyps ≤5 mm in the rectosigmoid colon untouched, or the resect-all group, where all polyps identified were removed regardless of optical assessment.
Randomization was stratified by sex, age category, and history of adenoma removal. Although endoscopists and patients were aware of treatment allocation (open-label), pathologists evaluating histology and outcome assessors remained blinded.
All colonoscopies utilized a combination of white light, blue light narrow band imaging, and computer-aided detection and diagnosis systems to characterize lesions. The primary endpoint was the adenoma detection rate (ADR), defined as the proportion of participants with at least one histologically confirmed adenoma detected, analyzed on an intention-to-treat basis. The study aimed to demonstrate non-inferiority of the leave-in-situ strategy with a 10% absolute margin.
Key Findings
Between October 2022 and April 2024, 1147 patients were enrolled; 895 patients (mean age 61.1 years, 57% female) were randomized to leave-in-situ (n=441) or resect-all (n=454) groups. Results showed 197 adenomas or colorectal cancers detected in the leave-in-situ arm versus 211 in the resect-all arm.
The ADR was 44.7% (95% CI 40.4 to 49.5) for the leave-in-situ group, compared with 46.5% (41.8 to 51.2) in the resect-all group. The absolute difference of -1.8 percentage points (95% CI -8.9 to 4.9) fulfilled the pre-specified non-inferiority criterion (p_non-inferiority=0.013), indicating that leaving small non-neoplastic polyps in situ guided by AI-assisted optical diagnosis did not compromise adenoma detection.
No colonoscopy-related adverse events, including bleeding or perforation, were reported in either cohort, underscoring the safety of this approach.
Expert Commentary
This landmark trial supports the clinical implementation of AI-assisted optical diagnosis for managing diminutive rectosigmoid polyps. The non-inferiority of adenoma detection rates between the leave-in-situ and resect-all strategies suggests that accurate AI-enhanced lesion characterization can allow endoscopists to avoid unnecessary polypectomies without compromising oncological safety.
By reducing unnecessary interventions, this approach may decrease procedure duration, risks of post-polypectomy complications, and healthcare costs. Moreover, it aligns well with precision medicine principles, tailoring intervention to lesion biology rather than size alone.
However, some limitations warrant consideration. The trial was conducted in highly experienced centers using the latest AI technologies, which might limit generalizability to community practice settings lacking such support. Additionally, longer-term clinical endpoints such as interval CRC incidence or adenoma recurrence were not assessed, representing important areas for future research.
Current guidelines emphasize optical diagnosis accuracy, but many practices have yet to adopt AI-assisted tools broadly. As AI systems become more accessible and endoscopists receive targeted training, adopting selective resection strategies may become the new standard.
Conclusion
The PRACTICE randomized trial demonstrates that an AI-assisted, optical diagnosis-based leave-in-situ strategy for small rectosigmoid colorectal polyps is non-inferior to routine polypectomy in terms of adenoma detection and safety. This evidence supports a paradigm shift towards more selective, less invasive colonoscopy management, potentially reducing unnecessary polypectomies and procedural risks without compromising cancer prevention.
Future studies should evaluate real-world implementation, cost-effectiveness, patient outcomes including long-term surveillance, and integration of emerging AI technologies.
References
1. Antonelli G, Desideri F, Scarozza P, et al. Safety of artificial intelligence-assisted optical diagnosis for leaving colorectal polyps in situ during colonoscopy (PRACTICE): a non-inferiority, randomised controlled trial. Lancet Gastroenterol Hepatol. 2025 Oct;10(10):915-923. doi: 10.1016/S2468-1253(25)00140-2. PMID: 40914178.
2. Hassan C, Rex DK, Wallace MB, et al. The role of artificial intelligence in endoscopy for the detection and characterization of colorectal polyps: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022;54(10):1049-1067. doi:10.1055/a-1765-4765.
3. Rex DK, Kahi C, O’Brien M, et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2015;81(1):31-53. doi:10.1016/j.gie.2014.06.033.
4. Kudo SE, Mori Y, Misawa M, et al. Artificial intelligence and colonoscopy: current status and future perspectives. Dig Endosc. 2021;33(6):951-961. doi:10.1111/den.13934.