Study Background and Disease Burden
Obesity remains a major global health challenge, contributing to elevated risks for cardiovascular disease, type 2 diabetes mellitus (T2DM), and reduced quality of life. Despite advances in behavioral and pharmacologic interventions, effective long-term obesity management continues to be a clinical unmet need. Existing therapies often require frequent dosing and exhibit modest weight loss efficacy or limiting adverse effects. Maridebart cafraglutide (MariTide) represents an innovative treatment modality combining glucagon-like peptide-1 receptor agonism (GLP-1 RA) with glucose-dependent insulinotropic polypeptide receptor antagonism (GIP RA), designed as a long-acting peptide-antibody conjugate administered once monthly. This dual incretin receptor targeting may exploit synergistic mechanisms influencing appetite regulation, insulin secretion, and energy metabolism, potentially yielding superior weight loss and metabolic benefits compared to current monotherapies.
Study Design
This investigation was a phase 2, double-blind, randomized, placebo-controlled, dose-ranging trial designed to evaluate the safety, tolerability, and efficacy of maridebart cafraglutide over 52 weeks. A total of 592 participants were enrolled and divided into two main cohorts: an obesity cohort (n=465) and an obesity with type 2 diabetes cohort (n=127).
Participants in the obesity cohort, with a mean BMI of 37.9 and mean age of 47.9 years, were randomized into seven maridebart cafraglutide treatment arms or placebo with varied dosing frequency, dose levels (140, 280, 420 mg), and dose escalation regimens. The obesity-diabetes cohort, characterized by a mean age of 55.1 years and mean BMI of 36.5, was randomized in a 1:1:1:1 ratio to three doses (140, 280, 420 mg) of maridebart cafraglutide or placebo, each administered every 4 weeks without dose escalation.
The primary efficacy endpoint was the percentage change in body weight from baseline to 52 weeks assessed via a treatment policy estimand, which follows an intention-to-treat framework. Secondary endpoints in the diabetes cohort included changes in glycated hemoglobin (HbA1c). Safety assessments included adverse event recording with particular focus on gastrointestinal tolerability.
Key Findings
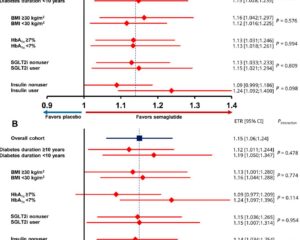
Maridebart cafraglutide induced substantial weight reduction across all dosing regimens compared to placebo. In the obesity cohort, weight loss ranged from -12.3% to -16.2%, significantly exceeding the placebo group’s -2.5% (95% confidence interval [CI] -4.2 to -0.7%). The highest dose regimen (420 mg every 4 weeks with dose escalation) was associated with the greatest mean weight loss reaching over 16% reduction at one year, a clinically meaningful magnitude rarely achieved with current obesity pharmacotherapies.
In the obesity-diabetes cohort, maridebart cafraglutide demonstrated weight reductions between -8.4% and -12.3%, versus -1.7% in placebo, alongside significant HbA1c improvements ranging from -1.2 to -1.6 percentage points, compared with a negligible change in placebo. These findings indicate robust dual metabolic benefits of maridebart cafraglutide on weight and glycemic control in patients with T2DM.
The safety profile was consistent with the known class effects of GLP-1 RAs. Gastrointestinal adverse events such as nausea, diarrhea, and vomiting were frequently observed but generally transient and less pronounced in regimens utilizing dose escalation and lower initial dosing. No unexpected safety signals or severe treatment-related adverse events were reported, underscoring a favorable tolerability profile supporting once-monthly administration.
Expert Commentary
The MariTide phase 2 trial offers compelling evidence that integrating GLP-1 receptor agonism with glucose-dependent insulinotropic polypeptide receptor antagonism can significantly enhance weight loss and glycemic control when compared with historical data on monotherapeutic agents. The magnitude of 16% mean weight loss is notable and approaches or surpasses that seen with bariatric surgery in some patients, albeit with a pharmacologic agent.
Clinical experts acknowledge that maridebart cafraglutide’s once-monthly administration enhances patient adherence potential, addressing a major barrier with daily or weekly injectable therapies. However, comparative trials with other approved GLP-1 RAs such as semaglutide or dual agonists like tirzepatide in a head-to-head setting are warranted to contextualize efficacy and safety.
Despite the positive findings, the study population comprised mostly middle-aged adults with relatively controlled comorbidities; extrapolation to older, multi-morbid populations or those with more severe diabetes requires caution. Long-term safety and cardiovascular outcome data remain crucial before broad clinical adoption.
Conclusion
Once-monthly maridebart cafraglutide represents a promising new pharmacotherapy for obesity management, demonstrating substantial and sustained weight loss in individuals with and without type 2 diabetes. The additional benefit of HbA1c reduction in diabetic patients underscores its potential dual utility. Gastrointestinal tolerability and the convenient dosing schedule favor patient compliance. Pending confirmatory phase 3 trials and long-term safety data, maridebart cafraglutide could significantly enhance the therapeutic armamentarium against obesity, addressing a vital unmet clinical need in a high-risk population.
References
1. Jastreboff AM, Ryan DH, Bays HE, Ebeling PR, Mackowski MG, Philipose N, Ross L, Liu Y, Burns CE, Abbasi SA, Pannacciulli N; MariTide Phase 2 Obesity Trial Investigators. Once-Monthly Maridebart Cafraglutide for the Treatment of Obesity – A Phase 2 Trial. N Engl J Med. 2025 Sep 4;393(9):843-857. doi: 10.1056/NEJMoa2504214. Epub 2025 Jun 23. PMID: 40549887.
2. Wilding JPH, Batterham RL, Calanna S, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021;384(11):989-1002.
3. Frias JP, Davies MJ, Rosenstock J, et al. Tirzepatide versus Semaglutide Once Weekly in Patients with Type 2 Diabetes. N Engl J Med. 2021;385(6):503-515.