Highlight
– Artificial intelligence (AI) demonstrated the capability to identify high-risk areas on screening mammograms suggestive of missed interval breast cancers (IBCs).
– AI detected numerous IBCs without visible abnormalities to radiologists on retrospective review, suggesting improved detection sensitivity.
– Women with high breast density, a known risk factor for screening challenges, were the focus, emphasizing clinical importance.
– AI scoring correlated with radiologists’ retrospective classifications, indicating complementary diagnostic value.
Study Background
Breast cancer remains a leading cause of cancer morbidity and mortality worldwide. Interval breast cancers (IBCs), diagnosed within 24 months following a normal screening mammogram, present a significant clinical challenge due to their aggressive nature and poorer outcomes compared to screen-detected cancers. High breast density, present in a substantial proportion of screening populations, obscures cancer detection on mammograms, increasing the likelihood of missed lesions. Current mammography screening programs (MSPs) often lack adjunctive tools to reliably identify these missed cancers early. Artificial intelligence applied to imaging analysis offers promise in augmenting radiologist performance by flagging subtle signs of malignancy undetected on initial human review.
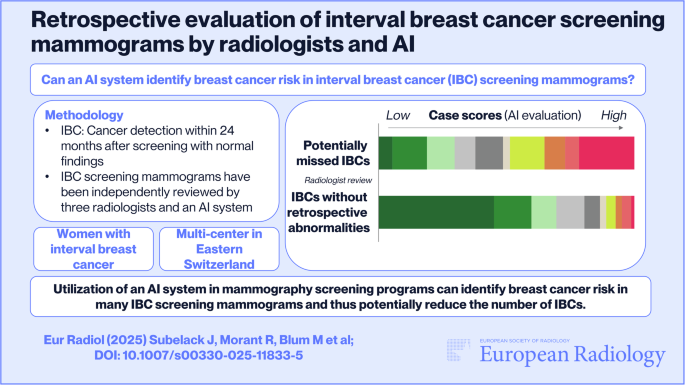
Study Design
This retrospective study analyzed 119 mammograms from women with a mean age of 57.3 years, predominantly exhibiting high breast density (BI-RADS categories c/d, 63.0%). Data was sourced from Eastern Switzerland and Grisons-Glarus cancer registries. Interval breast cancers were defined as invasive or in situ malignancies diagnosed within two years post a prior normal mammogram. Three radiologists independently performed retrospective reviews identifying visible abnormalities, categorizing lesions as potentially missed IBCs or IBCs without detectable retrospectively abnormalities based on consensus recommendations. An AI system evaluated each mammogram generating two scores on a 0–100 scale: a case score estimating current cancer presence likelihood and a risk score predicting breast cancer diagnosis probability within two years.
Key Findings
The analysis revealed that 68.9% of IBCs had no visible retrospective abnormalities per radiologists, while 31.1% were classified as potentially missed IBCs, with these receiving significantly higher BI-RADS scores (P < .05).
Potentially missed IBCs had a notably higher mean AI case score than those without retrospective abnormalities (54.1 vs 23.1; P < .05) and were more frequently assigned a higher risk category (48.7% vs 14.6%; P < .05).
Across all IBC cases, 46.2% had AI case scores over 25, 25.2% over 50, and 13.4% over 75, signifying varied AI-assessed malignancy likelihood.
Notably, potentially missed IBCs showed a broad distribution spanning low to high AI scores, while IBCs without retrospective abnormalities consistently scored low on both case and risk measures. Specifically, 73.0% of potentially missed IBCs versus 34.1% of IBCs without retrospective abnormalities had case scores exceeding 25; 51.4% versus 13.4% exceeded 50; and 29.7% versus 6.1% surpassed 75.
Expert Commentary
This study underscores AI’s added value in mammography, particularly in high breast density populations where conventional readings are limited. The AI system not only corroborated radiologists’ retrospective findings of missed malignancies but also unveiled a significant fraction of cancers invisible even upon expert second review.
Such findings advocate integrating AI as a clinical adjunct to reduce interval cancer rates, thereby improving early detection and potentially patient outcomes. However, limitations include the retrospective design, relatively small sample size, and predominance of high-density cases, which may impact generalizability. Prospective validation across broader populations and integration protocols in clinical workflow are necessary to confirm impact and operational feasibility.
Conclusion
Artificial intelligence demonstrates promising capability in detecting missed interval breast cancers on screening mammograms, particularly in women with dense breasts. By identifying cancers radiologists cannot retrospectively visualize, AI has the potential to enhance screening sensitivity, reduce delayed diagnoses, and optimize breast cancer management. Future studies should focus on prospective assessment, cost-effectiveness, and establishing standardized AI integration frameworks to realize these benefits in real-world mammography screening programs.
References
Eisemann N, Bunk S, Mukama T, Baltus H, Elsner SA, Gomille T, Hecht G, Heywang-Köbrunner S, Rathmann R, Siegmann-Luz K, Töllner T, Vomweg TW, Leibig C, Katalinic A. Nationwide real-world implementation of AI for cancer detection in population-based mammography screening. Nat Med. 2025 Mar;31(3):917-924. doi: 10.1038/s41591-024-03408-6 IF: 50.0 Q1 . Epub 2025 Jan 7. PMID: 39775040 IF: 50.0 Q1 ; PMCID: PMC11922743 IF: 50.0 Q1 .
PDF file download



