Highlight
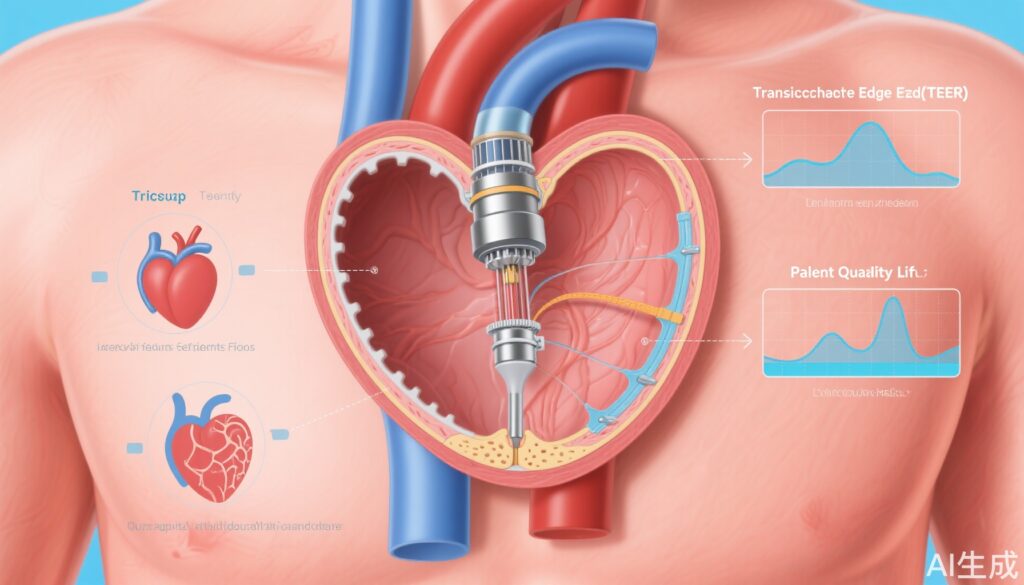
– Transcatheter edge-to-edge repair (TEER) significantly reduces the severity of severe tricuspid regurgitation (TR).
– TEER is associated with improved quality of life and reduced heart failure hospitalizations up to two years post-procedure.
– The procedure demonstrates a high safety profile with low rates of major adverse events.
– TEER is effective and safe even in patients with transvalvular cardiac implantable electronic device (CIED) leads.
Study Background and Disease Burden
Severe tricuspid regurgitation is a clinically debilitating condition characterized by backward flow of blood from the right ventricle into the right atrium during systole. This valvular pathology significantly contributes to symptoms of heart failure, reduced exercise capacity, and poor quality of life, particularly in the elderly population. Given the high morbidity and often late presentation, treatment options have traditionally been limited, with surgical interventions carrying elevated risks. Thus, minimally invasive therapies that can effectively reduce TR hold promise for improving clinical outcomes and patient well-being.
Study Design
The TRILUMINATE Pivotal Trial is a large, prospective, randomized controlled study designed to evaluate the safety and efficacy of percutaneous transcatheter edge-to-edge repair (TEER) for severe, symptomatic tricuspid regurgitation. Across 65 centers in the United States, Canada, and Europe, patients with symptomatic severe TR were randomized 1:1 to receive either the TEER procedure using the TriClip system plus medical therapy or medical therapy alone.
The primary hierarchical composite endpoint incorporated any-cause mortality or tricuspid valve surgery, hospitalization for heart failure, and a significant quality-of-life improvement measured by the Kansas City Cardiomyopathy Questionnaire (KCCQ). Improvement was defined as at least a 15-point increase at one year. Secondary endpoints assessed tricuspid regurgitation severity and procedural safety. Follow-up extended to two years for assessment of durability, hospitalizations, and survival.
Additionally, a subset analysis evaluated the safety and efficacy of TEER in patients with transvalvular CIED leads—a patient group known to pose technical challenges due to the presence of pacing or defibrillator leads crossing the tricuspid valve.
Key Findings
The initial report enrolled 350 patients (mean age 78, 54.9% female), equally divided between TEER and control groups. At one year, the TEER group demonstrated a statistically significant advantage in the primary composite endpoint with a win ratio of 1.48 (95% CI, 1.06–2.13; P=0.02). This was primarily driven by improvements in quality-of-life scores, with the TEER group experiencing a mean increase of 12.3 points in the KCCQ compared to 0.6 points in controls (P<0.001). Importantly, 87% of TEER recipients achieved TR reduction to moderate or less severity at 30 days versus only 4.8% of controls (P<0.001). Safety was confirmed, with 98.3% of TEER patients free from major adverse events at 30 days.
Two-year follow-up including an expanded cohort of 572 patients reaffirmed these benefits. The TEER group showed significantly fewer recurrent hospitalizations for heart failure (0.19 vs 0.26 events per patient-year; P=0.02). Freedom from all-cause mortality, tricuspid valve surgery, or additional valve interventions was markedly higher at 77.6% compared with 29.3% in controls (P<0.0001). Mortality and surgery rates were similar across groups, indicating TEER's role in reducing clinical deterioration rather than modifying survival at this timepoint. Importantly, 84% of TEER patients sustained moderate or less TR at two years, attesting to procedural durability.
In patients with transvalvular CIED leads (n=98), TEER demonstrated a comparable safety and efficacy profile to patients without such leads. Procedural success remained high, TR reduction rates at 30 days and one year were similar, and quality-of-life improvements were significant. No adverse impact was observed on CIED function, and procedural times were shorter overall, except for lead-induced TR cases. These findings expand the treatable patient population and support TEER’s feasibility in complex clinical scenarios.
Expert Commentary
The TRILUMINATE studies present a compelling case for TEER as a minimally invasive approach to severe TR, addressing an unmet clinical need often relegated to palliative management or high-risk surgery. The improvement in patient-centered outcomes such as quality of life and heart failure hospitalizations is particularly noteworthy.
Limitations include the relatively advanced age of participants and the predominance of functional TR cases, which may affect generalizability. Long-term survival benefit remains unproven, necessitating further studies with extended follow-up. Moreover, the hierarchical composite endpoint, while comprehensive, may dilute the interpretability of individual components, such as mortality and hospitalization rates.
Mechanistically, TEER’s ability to approximate valve leaflets reduces the regurgitant orifice, improving forward flow and right ventricular loading conditions, which plausibly underlies the clinical benefits observed.
Conclusion
Transcatheter edge-to-edge repair emerges as a safe, effective therapeutic option for patients with severe symptomatic tricuspid regurgitation, producing durable reduction in valvular incompetence, improved quality of life, and diminished heart failure hospitalizations over at least two years. Its proven safety in patients with transvalvular CIED leads expands its applicability. Ongoing research should focus on defining long-term survival impact, patient selection refinement, and extending treatment availability across diverse clinical settings.
References
Sorajja P, Whisenant B, Hamid N, et al. Transcatheter Repair for Patients with Tricuspid Regurgitation. N Engl J Med. 2023;388(20):1833-1842. doi:10.1056/NEJMoa2300525
Kar S, Makkar RR, Whisenant BK, et al. Two-Year Outcomes of Transcatheter Edge-to-Edge Repair for Severe Tricuspid Regurgitation: The TRILUMINATE Pivotal Randomized Controlled Trial. Circulation. 2025;151(23):1630-1638. doi:10.1161/CIRCULATIONAHA.125.074536
Naik H, Price MJ, Kapadia S, et al. Tricuspid Transcatheter Edge-to-Edge Repair in Patients With Transvalvular CIED Leads: The TRILUMINATE Pivotal Trial. JACC Clin Electrophysiol. 2025;11(5):1012-1020. doi:10.1016/j.jacep.2025.01.001