Highlight
- Smoking increases beneficial short-chain fatty acids like acetate and butyrate in UC patients, enhancing intestinal barrier integrity and anti-inflammatory effects.
- Smoking promotes colonization of oral bacteria, notably Streptococcus mitis, in the colonic mucosa of UC patients but triggers adverse immune responses in CD.
- In murine models, S. mitis colonization attenuates inflammation in UC but exacerbates disease in CD, partly via modulation of T helper 1 and CD8+ interferon-gamma producing T cells.
- Hydroquinone, an aromatic compound from cigarette smoke, facilitates oral bacterial colonization and could serve as a therapeutic mimic to harness smoking’s benefits without harmful effects.
Study Background and Disease Burden
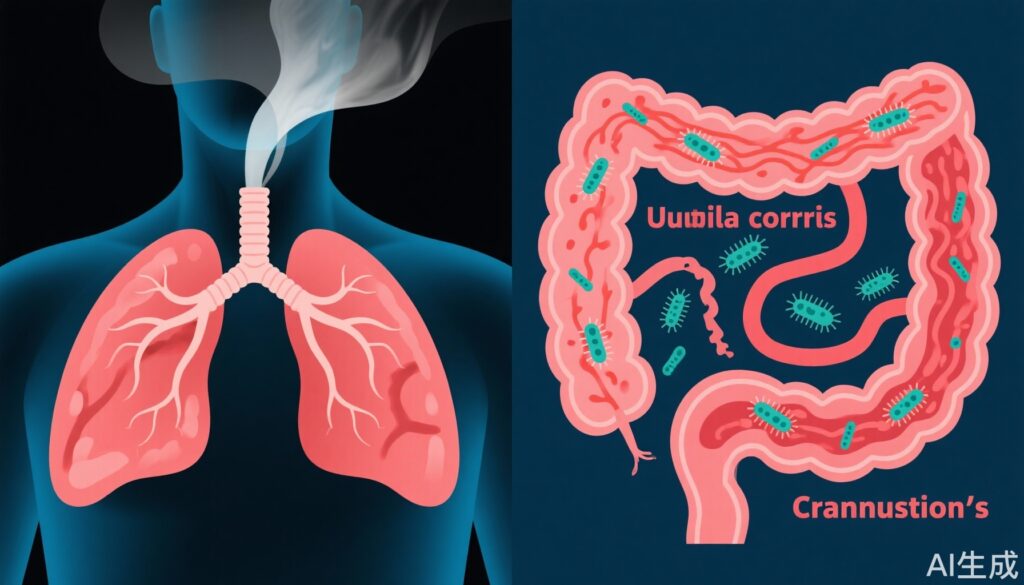
Inflammatory bowel disease (IBD) encompasses two major phenotypes: Crohn’s disease (CD) and ulcerative colitis (UC). Both are chronic, relapsing-remitting inflammatory disorders of the gastrointestinal tract, which impose considerable morbidity and healthcare burden worldwide. Interestingly, cigarette smoking—a well-known environmental risk factor for numerous diseases—exerts diametrically opposite effects on these two conditions. Smoking aggravates CD symptoms, disease progression, and postoperative recurrence, whereas it appears protective against UC onset and severity. This paradox has perplexed clinicians and researchers alike, with underlying mechanisms poorly understood.
Understanding how smoking influences gut immune homeostasis and microbiota could illuminate crucial pathogenic pathways and inform novel therapeutic strategies for these heterogeneous disorders. The current study by Miyauchi et al. provides new mechanistic insight into how smoking modulates metabolomic profiles and mucosal microbiota differently in UC versus CD, influencing intestinal immunity and disease outcomes.
Study Design
This investigation applied an integrative multi-omics and translational animal model approach. Researchers enrolled patients with IBD, stratified by diagnosis (UC or CD) and smoking status (never, former, or current smokers), alongside healthy controls. They collected saliva, fecal samples, and colonic mucosal biopsies to characterize bacterial profiles and metabolites.
Metabolomic profiling focused on identifying short-chain fatty acids (SCFAs) and aromatic compounds associated with smoking. Microbiome analyses delineated differences in oral and gut mucosal bacterial taxa, identifying key species differentially enriched among smokers with UC or CD.
To explore causality, the authors used germ-free mice colonized with identified oral bacteria, notably Streptococcus mitis. These mice were subjected to established murine models of UC and CD-like colitis to evaluate how bacterial colonization influences gut immune responses and inflammatory phenotypes.
Key Findings
The study uncovered critical molecular and microbial distinctions linked to smoking in UC and CD:
1. Increased short-chain fatty acids in UC smokers: Fecal analysis revealed that UC patients who smoked exhibited significantly elevated levels of major SCFAs, particularly acetate and butyrate, compared to former smokers. SCFAs are potent anti-inflammatory metabolites that preserve epithelial barrier function and regulate immune tolerance. Though similar trends were noted in CD smokers, limited patient numbers weakened statistical certainty in this group.
2. Smoking-induced presence of aromatic tobacco components: Hydroquinone and related compounds were notably raised in feces of UC smokers. These aromatic compounds correlated with increased colonization of mouth-origin bacteria in the colonic mucosa.
3. Oral bacteria infiltration in the gut mucosa: Streptococcus mitis, an oral commensal, was significantly enriched in the colonic mucosa of UC smokers, suggesting that cigarette smoke compounds promote oral bacterial translocation and persistence in the colon.
4. Immune modulation by Streptococcus mitis colonization: Germ-free mice colonized with S. mitis showed differential immune effects: in UC models, colonization increased T helper type 1 and interferon-gamma producing CD8+ T cells, which paradoxically attenuated inflammation; conversely, in CD models, the same immune profile worsened colitis severity.
5. Potential therapeutic implications: The data suggest that the protective effect of smoking against UC is mediated through gut colonization by Streptococcus species and their immune-modulatory effects, possibly facilitated by hydroquinone. This raises prospects for microbiota- or metabolite-based therapies mimicking smoking’s benefits without its well-known systemic harms.
Expert Commentary
Dr. Hiroshi Ohno, lead author from RIKEN Center for Integrative Medical Sciences, commented, “Our findings elucidate a novel gut immunological axis wherein oral bacteria relocation, promoted by cigarette smoke-derived compounds, differentially modulate UC and CD. Harnessing these mechanisms could transform IBD management by enabling targeted bacterial or metabolite therapies.”
However, limitations temper the conclusions. The relatively small CD cohort, owing to lower CD prevalence in Japan, restricts extrapolation for this disease. Murine colitis models do not fully replicate human IBD’s chronicity and complex epithelial barrier dysfunction. Additionally, medication history and timing since last flare were not comprehensively captured, potentially confounding results.
Existing evidence linking smoking to microbiome alterations complements this study’s findings, underscoring the multifaceted role of environmental factors in shaping IBD pathogenesis. Nonetheless, clinical translation awaits validation in larger, diverse cohorts and longer-term mechanistic studies.
Conclusion
This pioneering research advances our understanding of why smoking paradoxically benefits UC while aggravating CD. By identifying distinct gut microbial and metabolomic signatures influenced by smoking, particularly the role of Streptococcus mitis and hydroquinone, it reveals mechanisms underpinning differential immune modulation in these diseases.
These insights open avenues for innovative, microbiota-targeted therapies that could emulate smoking’s beneficial effects for UC patients without the toxic risks of tobacco exposure. Future studies should aim to confirm these findings in broader populations, refine microbial or metabolite interventions, and explore integration into personalized IBD treatment algorithms.
References
Miyauchi E, Taida T, Uchiyama K, Nakanishi Y, Kato T, Koido S, Sasaki N, Ohkusa T, Sato N, Ohno H. Smoking affects gut immune system of patients with inflammatory bowel diseases by modulating metabolomic profiles and mucosal microbiota. Gut. 2025 Aug 25:gutjnl-2025-334922. doi: 10.1136/gutjnl-2025-334922. Epub ahead of print. PMID: 40854688.