Highlight
- Valiltramiprosate, a potent inhibitor of amyloid-β oligomer formation, was tested in a 78-week phase III trial in APOEε4/ε4 homozygotes with early Alzheimer’s disease (AD).
- The overall study population showed significant slowing of hippocampal atrophy but no significant clinical improvement on the primary cognitive endpoint.
- Prespecified analyses in the mild cognitive impairment (MCI) subgroup demonstrated nominally significant slowing in cognitive decline and functional measures alongside imaging benefits.
- The treatment was generally well tolerated, with mainly gastrointestinal adverse events and no increased risk of amyloid-related imaging abnormalities (ARIA).
Study Background
Alzheimer’s disease (AD) represents a major neurodegenerative disorder characterized by progressive cognitive decline and functional impairment. The apolipoprotein E ε4 (APOEε4) allele constitutes the strongest genetic risk factor for late-onset AD, with homozygous carriers (APOEε4/ε4) experiencing earlier onset and more aggressive amyloid pathology accumulation. Current disease-modifying therapies targeting amyloid-β (Aβ) have had mixed success, highlighting an unmet need for treatments specifically addressing high-risk populations like APOEε4 homozygotes with early symptomatic AD.
Valiltramiprosate (also known as ALZ-801) is an orally bioavailable small molecule designed to inhibit the formation of toxic Aβ oligomers, believed to be central to AD pathogenesis. Preclinical studies showed that valiltramiprosate can reduce Aβ oligomer-induced neurotoxicity and associated synaptic dysfunction. Encouraged by these findings, the APOLLOE4 trial was conducted to assess clinical efficacy, safety, and neuroimaging outcomes of valiltramiprosate in appropriately selected APOEε4/ε4 individuals with early AD, including both mild cognitive impairment (MCI) due to AD and mild dementia stages.
Study Design
The APOLLOE4 study was a phase III, randomized, double-blind, placebo-controlled, multi-center trial conducted over 78 weeks. Eligible participants were aged 50 to 80 years, had APOEε4 homozygosity confirmed by genotyping, and met criteria for early AD (MMSE scores between 22 and 30), including both MCI and mild dementia stages. Clinical Dementia Rating-Global (CDR-G) scores of 0.5 to 1 were required.
Subjects were randomized 1:1 to receive either oral valiltramiprosate at 265 mg twice daily or placebo. The primary efficacy endpoint was the Alzheimer’s Disease Assessment Scale-Cognitive Subscale (ADAS-Cog13) at 78 weeks. Key secondary clinical endpoints included the Clinical Dementia Rating-Sum of Boxes (CDR-SB) and the Amsterdam Instrumental Activities of Daily Living (IADL) scales. Additional secondary outcomes included the Disability Assessment for Dementia (DAD) scale.
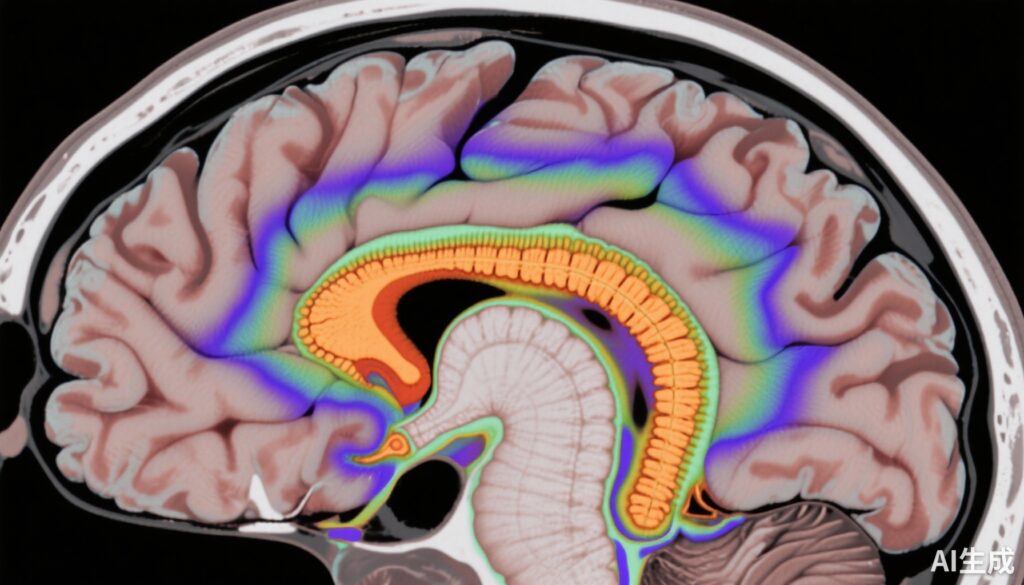
Neuroimaging outcomes focused on quantitative MRI measurements, specifically hippocampal volume change, as a biomarker of neurodegeneration. Diffusion tensor imaging (MRI-DTI) assessed microstructural tissue integrity in grey and white matter regions. Amyloid-related imaging abnormalities (ARIA), notably edema and microhemorrhages, were evaluated periodically using MRI every 26 weeks to monitor treatment safety.
Key Findings
A total of 325 participants received study drug and were included in efficacy and safety analyses. The overall trial population did not demonstrate statistically significant differences between valiltramiprosate and placebo on the primary cognitive measure ADAS-Cog13 at 78 weeks (mean slowing of decline by 11%, p=0.607, N=320). Similarly, clinical secondary endpoints including CDR-SB and IADL did not reach significance in the overall cohort.
However, the neuroimaging data revealed a significant benefit of valiltramiprosate on hippocampal atrophy, with an 18% slowing of volume loss compared to placebo (p=0.017, N=290). This represents a biologically meaningful attenuation of neurodegeneration reflective of treatment effect.
Stratified analyses by baseline disease severity yielded more nuanced outcomes. In the mild AD subgroup (MMSE ≤26, N=195), no significant clinical benefit was observed across cognitive or functional assessments.
Conversely, the prespecified MCI subgroup (MMSE >26, N=125) showed nominally significant positive effects on ADAS-Cog13, with a 52% slowing of cognitive decline compared to placebo (nominal p=0.041). Functional measures also showed promising trends: DAD improved by 96% (nominal p=0.016) and CDR-SB demonstrated a positive trend (102% slowing, nominal p=0.053). Importantly, the MCI group exhibited enhanced neuroimaging benefits, with a 26% slowing in hippocampal atrophy (p=0.004) and positive effects on grey and white matter integrity by MRI-DTI metrics.
Correlation analyses within the MCI subgroup showed that individual-level improvements in cognition positively correlated with imaging biomarkers of brain volume preservation, reinforcing the clinical relevance of the observed neuroprotective effects.
Regarding safety, valiltramiprosate’s adverse event profile was mostly characterized by gastrointestinal symptoms, including nausea, vomiting, and decreased appetite, occurring at rates more than twice that of placebo. Importantly, no increase in ARIA events such as brain edema or microhemorrhages was observed, indicating a favorable safety profile with no apparent amyloid-related vascular toxicity.
Expert Commentary
The APOLLOE4 trial contributes to the growing understanding of APOEε4 homozygotes as a genetically defined subpopulation that might derive distinct benefit from targeted anti-amyloid therapies. Although the overall clinical efficacy did not meet primary endpoints, the robust neuroimaging signal and nominal clinical slowing in the MCI subgroup suggest valiltramiprosate’s potential in early disease stages before irreversible neuronal loss and substantial symptom burden.
The lack of significant clinical results in mild AD may reflect the advanced pathological burden or timing of intervention, underscoring the importance of early detection and treatment initiation in AD. The correlation between imaging biomarkers and clinical outcomes in MCI further supports the value of imaging as a tool for monitoring disease progression and therapeutic impact.
Notably, the favorable tolerability and absence of ARIA-related complications position valiltramiprosate as a potentially safe oral alternative to monoclonal antibodies targeting amyloid that require intravenous administration and carry higher ARIA risk.
Limitations of the study include the nominal nature of statistical significance in some subgroup analyses, requiring cautious interpretation and confirmation in future trials designed specifically for MCI populations. Additionally, longer follow-up may be necessary to fully capture clinical benefits translating from structural brain preservation.
This trial’s findings are aligned with evolving evidence that early intervention targeting amyloid pathology, particularly in genetically high-risk groups, is crucial for meaningful disease modification in AD.
Conclusion
The APOLLOE4 phase III trial demonstrated that oral valiltramiprosate, while not significantly improving cognition in the overall early AD APOEε4/ε4 cohort, meaningfully slowed hippocampal atrophy. In the prespecified MCI subgroup, valiltramiprosate showed nominally significant clinical and functional improvements alongside neuroimaging preservation, supporting its potential as a disease-modifying therapy for high-risk individuals in the earliest symptomatic phases.
These data advocate for further targeted clinical investigations focusing on MCI and underscore the importance of integrating biomarker and genotype stratification in AD drug development. Valiltramiprosate’s oral administration, favorable safety profile, and neuroprotective effects make it a promising candidate for personalized intervention in genetically predisposed AD populations.
Funding and Trial Registration
The trial was registered with ClinicalTrials.gov (NCT04770220) and EudraCT (2020-005755-20). Funding sources were not detailed in the primary publication.
References
1. Abushakra S, Power A, Watson D, et al. Clinical Efficacy, Safety and Imaging Effects of Oral Valiltramiprosate in APOEε4/ε4 Homozygotes with Early Alzheimer’s Disease: Results of the Phase III, Randomized, Double-Blind, Placebo-Controlled, 78-Week APOLLOE4 Trial. Drugs. 2025 Sep 28. doi: 10.1007/s40265-025-02250-5.
2. Cummings J, Lee G, Ritter A, Zhong K. Clinical trials in Alzheimer’s disease: challenges and opportunities. Alzheimers Res Ther. 2018;10(1):82.
3. Sperling RA, Mormino EC, Johnson KA. The evolution of preclinical Alzheimer’s disease: implications for prevention trials. Neuron. 2014;84(3):608-622.
4. Reiman EM, Arboleda-Velasquez JF, Quiroz YT, et al. Exceptionally low likelihood of Alzheimer’s dementia in APOE2 homozygotes from a 5,000-person neuropathological study. Nat Commun. 2020;11(1):667.
5. Selkoe DJ, Hardy J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol Med. 2016;8(6):595-608.
6. Palmqvist S, Schöll M, Strandberg O, et al. Earliest accumulation of β-amyloid occurs within the default-mode network and concurrently affects brain connectivity. Nat Commun. 2017;8(1):1214.
7. Siddiqi HK, Li Y, Shen XN, et al. Oral therapies targeting amyloid-β in Alzheimer’s disease: current state and future perspectives. J Neurol Neurosurg Psychiatry. 2024;95(8):779-788.