Study Background and Disease Burden
Obesity is a chronic, relapsing disease associated with increased risks of cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality. Globally, its prevalence is rising, including in Asian countries where the health consequences of obesity manifest at lower body mass indexes (BMIs) relative to Western populations. Recognizing this, the World Health Organization (WHO) recommends defining obesity in many Asian populations at BMI ≥25 kg/m², rather than ≥30 kg/m² as is standard in other ethnic groups. This adaptation accounts for the disproportionate cardiometabolic risk seen among Asians at these lower BMI thresholds.
Despite lifestyle intervention being the cornerstone of obesity management, pharmacotherapy often plays a key role in achieving significant weight loss. Semaglutide, a glucagon-like peptide-1 receptor agonist (GLP-1 RA), has demonstrated robust efficacy in weight reduction among diverse populations but data specific to Asian cohorts with obesity (BMI ≥25 kg/m²) without diabetes are sparse. The STEP 11 trial was thus designed to address this unmet clinical need by evaluating the efficacy and safety of once-weekly subcutaneous semaglutide 2.4 mg combined with lifestyle intervention in adults from South Korea and Thailand living with obesity.
Study Design
STEP 11 was a 44-week, randomized, double-blind, placebo-controlled phase 3 trial conducted across 12 clinical sites in South Korea and Thailand. Adults aged ≥18 years in Thailand and ≥19 years in South Korea, of Asian descent, with a BMI ≥25 kg/m² and without diabetes, were enrolled.
Participants were randomized in a 2:1 ratio to receive either once-weekly subcutaneous semaglutide 2.4 mg or placebo. Both arms incorporated standardized lifestyle interventions comprising a reduced-calorie diet and increased physical activity. The randomization sequence was computer-generated, employing block randomization. Blinding was maintained for participants, care providers, investigators, and outcome assessors.
The coprimary endpoints were: (1) percentage change in body weight from baseline to week 44, and (2) proportion of participants achieving ≥5% bodyweight reduction at week 44, analyzed on an intention-to-treat (ITT) basis. Confirmatory secondary endpoints included proportions of participants achieving ≥10% and ≥15% bodyweight reduction and the mean change in waist circumference. Safety and tolerability were monitored by adverse event surveillance among all participants who received at least one dose of the investigational agent or placebo.
This trial was registered under ClinicalTrials.gov identifier NCT04998136.
Key Findings
Between August 15, 2022, and November 20, 2023, a total of 150 participants were randomized: 101 to semaglutide 2.4 mg and 49 to placebo. The median demographic profile included a mean age of 39 years, 74% female representation, mean baseline weight of 83.8 kg, and mean BMI 31.3 kg/m².
Treatment adherence was high with only 6% in the semaglutide arm and 4% in placebo discontinuing prematurely.
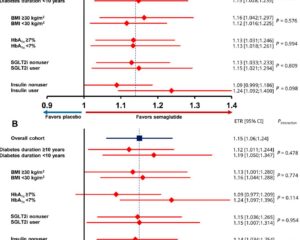
The semaglutide-treated group exhibited a statistically significant mean reduction in body weight of 16.0% (SE 0.7), compared to 3.1% (SE 0.9) in the placebo group (p<0.0001). Correspondingly, 96% of the semaglutide group achieved ≥5% weight reduction versus 25% in placebo (p<0.0001). Likewise, weight loss thresholds of ≥10% and ≥15% were reached by 78% and 53% in the semaglutide cohort, compared to 10% and 4.2% in placebo (both p<0.0001).
Waist circumference decreased by a mean of 11.9 cm in the semaglutide group versus 3.0 cm in placebo (p<0.0001), supporting a significant reduction in central adiposity.
Concerning safety, adverse events (AEs) were reported in 89% of semaglutide recipients and 78% of placebo recipients. Most commonly reported AEs in the semaglutide arm were gastrointestinal, including nausea, vomiting, and diarrhea, consistent with the known GLP-1 receptor agonist profile. Serious adverse events occurred in 13% of semaglutide users compared to 8% with placebo; the specific nature of these events was not detailed in the summary but warrants further scrutiny. Overall, semaglutide was generally well tolerated.
Expert Commentary
The STEP 11 trial extends prior evidence from global semaglutide studies to an Asian population where obesity definitions and associated risks differ. This study’s demonstration of robust efficacy and tolerability of semaglutide in Asians with BMI ≥25 kg/m² fills a critical data gap. The magnitude of weight loss is clinically meaningful and comparable to results seen in higher BMI Western cohorts. Given the disproportionate cardiometabolic risks Asians face even at lower BMI strata, early and effective pharmacologic intervention is prudent.
Nonetheless, the trial is limited by a relatively small sample size and short-term follow-up duration. Longer studies examining durability of weight loss, cardiovascular outcomes, and rare adverse events in Asian populations are desirable. Moreover, the predominance of female participants (74%) may limit generalizability to males. Biological mechanisms underlying enhanced semaglutide responsiveness in this population remain to be elucidated, though GLP-1 receptor agonists are known to mediate appetite suppression and improved glycemic regulation.
From a policy perspective, STEP 11 supports updating local clinical guidelines in Asian countries to incorporate semaglutide 2.4 mg for obesity management at the defined BMI thresholds. Payer reimbursement considerations should reflect the cost-effectiveness of weight reduction in reducing downstream metabolic complications in this context.
Conclusion
The STEP 11 randomized controlled trial confirms that once-weekly semaglutide 2.4 mg combined with lifestyle modification leads to significant and clinically relevant weight loss among Asian adults with obesity defined by BMI ≥25 kg/m², without diabetes. The safety profile aligns with previous studies and is acceptable in clinical practice. These findings hold important implications for both clinical management and health policy in Asian populations, emphasizing the need for tailored obesity treatment algorithms that consider ethnic-specific BMI cutoffs and risk profiles.
Continued research is warranted to evaluate long-term outcomes, mechanistic pathways, and real-world effectiveness to optimize obesity care in diverse populations.
References
1. Lim S, Buranapin S, Bao X, Quiroga M, Park KH, Kang JH, Rinnov AR, Suwanagool A. Once-weekly semaglutide 2·4 mg in an Asian population with obesity, defined as BMI ≥25 kg/m2, in South Korea and Thailand (STEP 11): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol. 2025 Aug 14:S2213-8587(25)00164-0. doi: 10.1016/S2213-8587(25)00164-0. Epub ahead of print. PMID: 40825340.
2. World Health Organization Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157-163.
3. Wilding JPH, Batterham RL, Calanna S, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021;384(11):989-1002.
4. Rubino D, Abrahamsson N, Davies M, et al. Effect of Continued Weekly Subcutaneous Semaglutide vs Placebo on Weight Loss Maintenance in Adults With Overweight or Obesity: The STEP 4 Randomized Clinical Trial. JAMA. 2021;325(14):1414-1425.