Highlight
- The PROLABI trial tested lung-protective ventilation in acute brain injury patients, comparing low tidal volume and higher PEEP to conventional methods.
- Contrary to expectations, the lung-protective strategy did not improve the composite primary outcome, and was associated with increased mortality and ventilator dependency.
- The incidence of ARDS was not significantly different between groups, and neurological outcomes showed no benefit from lung-protective ventilation.
- Early trial termination limits definitive conclusions, warranting larger trials to confirm safety and efficacy in this vulnerable population.
Study Background and Disease Burden
Patients with severe acute brain injury frequently require mechanical ventilation due to impaired consciousness and airway protection. Ventilation strategies are crucial in this context, as they affect both pulmonary and cerebral physiology. Lung-protective ventilation, characterized by lower tidal volumes (VT) and moderate positive end-expiratory pressure (PEEP), has become standard care for critically ill patients due to its benefits in reducing ventilator-induced lung injury and acute respiratory distress syndrome (ARDS). However, in patients with acute brain injury, the application of lung-protective strategies remains controversial. Concerns stem from the potential adverse effects of higher PEEP on intracranial pressure and cerebral perfusion as well as challenges in maintaining optimal carbon dioxide levels, which are critical for cerebral hemodynamics. Previously, no large interventional trials have evaluated the impact of lung-protective ventilation in this specific population, creating a major clinical knowledge gap.
Study Design
The PROLABI trial was a multicenter, open-label, randomized controlled clinical trial conducted to compare lung-protective ventilation versus conventional ventilation in adult patients with severe acute brain injury. A total of 190 patients were enrolled across multiple intensive care units and randomly assigned to receive either a lung-protective ventilation strategy—with lower tidal volumes and higher PEEP—or a conventional ventilatory protocol.
The primary endpoint was a composite of death, ventilator dependency, and development of ARDS within 28 days of randomization. Secondary outcomes included neurological status assessed by the Oxford Handicap Scale at ICU discharge and the Glasgow Outcome Scale at 6 months post-injury. The trial followed an intention-to-treat analysis. The study was prematurely stopped due to funding discontinuation after enrolling 190 subjects, below the initially planned sample size.
Key Findings
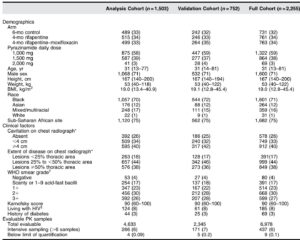
Baseline characteristics were well-balanced between the lung-protective and conventional ventilation groups.
– The composite primary outcome occurred in 61.5% of patients in the lung-protective group versus 45.3% in the conventional group (Relative Risk [RR] 1.35; 95% Confidence Interval [CI], 1.03 to 1.79; P=0.025), indicating a worse outcome associated with lung-protective ventilation.
– Mortality was significantly higher in the lung-protective group at 28.9% compared to 15.1% in the conventional group (RR 1.91; 95% CI, 1.06 to 3.42; P=0.02).
– Ventilator dependency was also increased in the lung-protective arm at 42.3% compared to 27.9% in the conventional arm (RR 1.52; 95% CI, 1.01 to 2.28; P=0.039).
– Incidence of ARDS did not differ significantly, occurring in 30.8% versus 22.1% of patients in the lung-protective and conventional groups, respectively (RR 1.39; 95% CI, 0.85 to 2.27; P=0.179).
– Neurological outcomes at ICU discharge and 6 months showed no significant differences between approaches.
The safety profile highlighted concerns surrounding lung-protective ventilation in this context, potentially related to its impact on cerebral physiology and gas exchange.
Expert Commentary
The PROLABI trial provides the first rigorous clinical trial evidence addressing lung-protective ventilation in patients with severe acute brain injury, challenging assumptions extrapolated from general critical care. The unexpected higher mortality and ventilator dependency rates associated with the lung-protective strategy contrast with findings in ARDS and heterogeneous ICU populations where such protocols are beneficial.
Potential explanations include the sensitivity of injured brain tissues to alterations in carbon dioxide tension and cerebral perfusion caused by low VT and higher PEEP. Increased intrathoracic pressure may compromise cerebral venous return and elevate intracranial pressure, negatively impacting neurologic recovery. Furthermore, controlling PaCO2 within a narrow therapeutic window is essential to avoid cerebral ischemia or hyperemia, a goal that might be more difficult to achieve with lung-protective settings.
Limitations of the trial include its early termination, which reduced statistical power, and the open-label design possibly introducing bias. The heterogeneity of brain injury types and severity could have also influenced outcomes. More detailed mechanistic studies monitoring intracranial pressure and cerebral hemodynamics during ventilation are needed to elucidate biological plausibility.
Current clinical guidelines recommend individualized ventilation with careful cerebral monitoring in brain-injured patients. This trial highlights that lung-protective ventilation cannot be assumed safe or beneficial without robust supportive data in this subgroup.
Conclusion
The PROLABI randomized clinical trial suggests that lung-protective ventilation with low tidal volume and moderate PEEP does not improve outcomes in patients with severe acute brain injury and may be associated with increased mortality and ventilator dependence. The incidence of ARDS did not differ significantly, and no neurological outcome benefit was observed.
Given the trial’s premature ending and limited sample size, these findings should be viewed as preliminary. They underscore the complexity of ventilatory management in neurocritical care and the need for large-scale, dedicated trials incorporating cerebral physiology monitoring to define optimal strategies.
Until further evidence emerges, mechanical ventilation in acute brain injury patients should carefully balance protective lung goals against potential cerebral hemodynamic risks, guided by individualized monitoring and interdisciplinary expertise.
References
Mascia L, Fanelli V, Mistretta A, Filippini M, Zanin M, Berardino M, Mazzeo AT, Caricato A, Antonelli M, Della Corte F, Grossi F, Munari M, Caravello M, Alessandri F, Cavalli I, Mezzapesa M, Silvestri L, Casartelli Liviero M, Zanatta P, Pelosi P, Citerio G, Filippini C, Rucci P, Rasulo FA, Tonetti T. Lung-Protective Mechanical Ventilation in Patients with Severe Acute Brain Injury: A Multicenter Randomized Clinical Trial (PROLABI). Am J Respir Crit Care Med. 2024 Nov 1;210(9):1123-1131. doi:10.1164/rccm.202402-0375OC. PMID:39288368.