Highlight
1. Lung cancer screening with low-dose computed tomography (LDCT) reduces mortality but remains underutilized in the US, with screening rates below 20% among eligible populations.
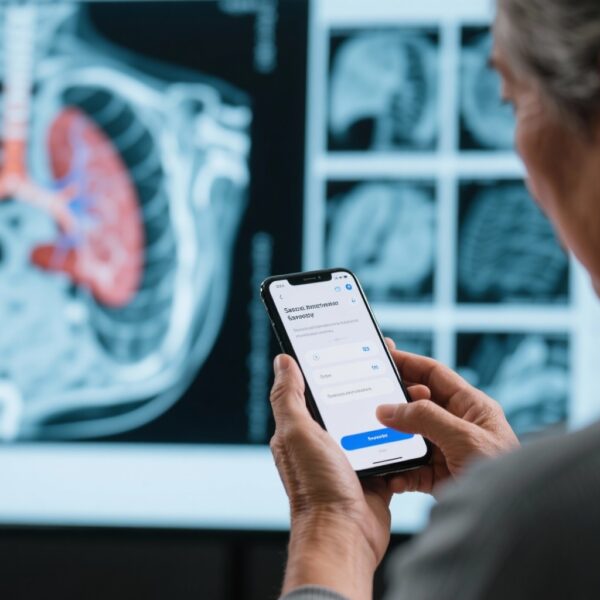
2. A randomized clinical trial investigating a direct-to-patient digital health program (mPATH-Lung) demonstrated a significant increase in lung cancer screening completion compared to enhanced usual care.
3. The intervention, deploying a decision aid and convenient option to request screening appointments outside clinical visits, showed good safety with minimal invasive procedures and no complications.
4. These findings support digital health approaches to overcome barriers in lung cancer screening uptake and highlight the need for broader implementation studies in diverse populations.
Study Background
Lung cancer remains the leading cause of cancer-related mortality worldwide. Early detection through screening with low-dose chest computed tomography (LDCT) has been shown to reduce lung cancer mortality among high-risk individuals, particularly heavy smokers aged 50–77 years. Despite robust clinical evidence and guideline recommendations, lung cancer screening uptake in the United States is dismally low, with less than 20% of eligible individuals undergoing screening. This is attributed to multiple factors including lack of patient awareness, limited access, and missed opportunities during healthcare visits.
Innovations in digital health offer potential routes to engage patients directly, providing education and facilitating shared decision-making without the constraints of in-person encounters. The mPATH-Lung program represents a direct-to-patient digital intervention designed to increase screening adherence by combining brief educational components, decision aids, and streamlined appointment request features.
Study Design
This randomized clinical trial was conducted between April 2022 and May 2023 at two academic health systems in the southeastern United States. The study enrolled individuals aged 50 to 77 years who met Centers for Medicare & Medicaid Services (CMS) criteria for lung cancer screening eligibility.
Participants (n=1,333) were randomized 1:1 to either the mPATH-Lung digital health program or enhanced usual care. The intervention group (n=669) received an emailed invitation to access the digital program which contained a brief decision aid about lung cancer screening and an option to request a screening appointment online outside of a clinical visit. The control group (n=664) received notification of their eligibility and was advised to discuss screening with their primary care clinician, consistent with enhanced usual care.
The primary endpoint was completion of any chest CT scan within 16 weeks post-intervention. Secondary outcomes encompassed screening decisions, process measures (screening visits, number of CT scans ordered), clinical outcomes (including lung cancer screening results and cancers diagnosed), screening-related harms, and implementation parameters.
Key Findings
Among 26,909 individuals identified by smoking history in electronic health records, 3,267 completed an initial eligibility questionnaire online and 1,333 qualified and consented for study participation. The population had a mean age of 60.7 years, was predominantly female (65%), and racially comprised 17% Black and 79% non-Hispanic White individuals. Insurance status was fairly balanced between commercial (47%) and public (45%) coverage.
Lung cancer screening completion measured by chest CT was significantly higher in the mPATH-Lung group at 24.5% (164/669) versus 17.0% (113/664) in the control group. This corresponds to an odds ratio of 1.6 (95% CI, 1.2–2.1), reflecting a 60% increased likelihood of screening completion with the digital intervention.
Regarding safety outcomes, among participants who completed LDCT, false-positive rates were 12.7% in the intervention arm and 8.4% in controls. Invasive diagnostic procedures were infrequent (2.0% intervention vs 1.1% control) and notably without complications, indicating the intervention did not increase harm.
Secondary process outcomes showed that the mPATH-Lung program facilitated more screening visits and CT orders, confirming the intervention’s role in driving care delivery rather than merely patient interest. Additionally, the program’s direct-to-patient design bypassed typical clinical visit barriers and may have resulted in increased engagement among diverse demographics.
Expert Commentary
The trial by Miller et al. addresses a critical gap in lung cancer prevention—the low uptake of proven screening modalities despite availability and guidelines. By leveraging digital health technology outside traditional visits, the study demonstrates a scalable strategy to enhance screening rates. The 60% improvement in CT completion is clinically meaningful and may translate into earlier lung cancer detection and better outcomes if implemented widely.
However, the study population, while racially mixed, was drawn from academic centers within a specific US region and may not fully represent nationwide patient populations or patients with limited digital literacy or internet access. The relatively modest absolute increase suggests further refinements and integration with healthcare systems might improve effectiveness. Additionally, the balance of screening benefits and harms must be carefully communicated, given the observed false-positive rates.
This work aligns with emerging guidelines endorsing shared decision-making and patient-centered approaches in lung cancer screening and underscores the need to incorporate digital tools thoughtfully. Further research should also evaluate cost-effectiveness, health equity considerations, and long-term clinical outcomes.
Conclusion
This randomized clinical trial confirms that a direct-to-patient digital health program significantly increases lung cancer screening completion among high-risk individuals compared to enhanced usual care. The intervention is safe, patient-friendly, and addresses gaps in the current screening paradigm, which could contribute to reducing lung cancer mortality through earlier detection. Future studies should focus on tailoring digital interventions across diverse populations and different healthcare settings to maximize reach and impact.
Funding and ClinicalTrials.gov Registration
The trial was registered under ClinicalTrials.gov Identifier: NCT04083859. Detailed funding disclosures were not provided in the source article.
References
Miller DP, Snavely AC, Dharod A, et al. A Direct-to-Patient Digital Health Program for Lung Cancer Screening: A Randomized Clinical Trial. JAMA. 2025 Oct 20. doi:10.1001/jama.2025.17281. PMID: 41114973.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Lung Cancer Screening (Version 3.2023).
Mazzone PJ, Silvestri GA, Patel S, et al. Screening for Lung Cancer: CHEST Guideline and Expert Panel Report. Chest. 2021 May;159(5):1776-1794.