Highlight
Adaptive deep brain stimulation (aDBS) dynamically adjusts stimulation based on real-time neural feedback, offering potential improvements over continuous DBS (cDBS) in Parkinson’s disease (PD). In a pivotal international trial, long-term at-home use of personalized aDBS was shown to be safe and effective in patients stable on cDBS. Both single and dual threshold aDBS modes met performance goals for increased symptom-controlled on-time without troublesome dyskinesias, with reduced energy delivery and minimal adverse effects.
Study Background and Disease Burden
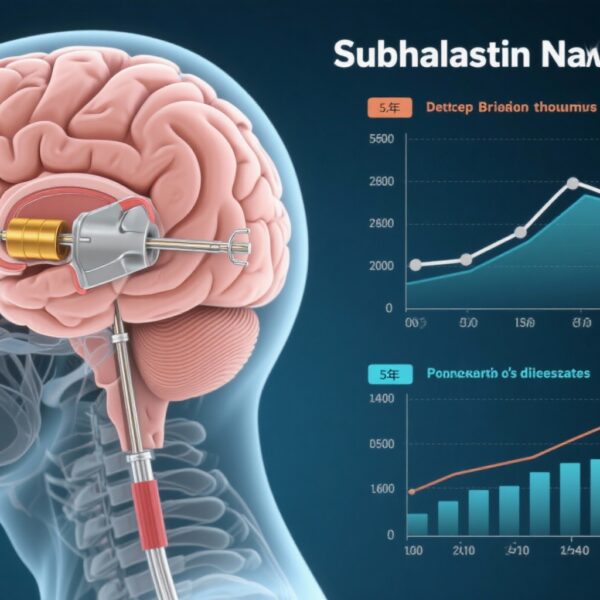
Parkinson’s disease is a progressive neurodegenerative disorder characterized by motor symptoms such as bradykinesia, rigidity, resting tremor, and postural instability, often accompanied by dyskinesias from levodopa therapy. Deep brain stimulation (DBS) targeting subthalamic nucleus or globus pallidus internus has become a mainstay for advanced PD refractory to medication, improving motor function and quality of life. However, traditional continuous DBS (cDBS) delivers fixed high-frequency stimulation irrespective of symptom fluctuations, potentially leading to side effects, suboptimal efficacy, and higher energy consumption.
Adaptive DBS (aDBS) utilizes closed-loop technology that adjusts stimulation amplitude in response to neural biomarkers—such as local field potentials—reflecting patients’ current motor states. This personalized approach aims to optimize therapeutic effects, reduce adverse events, and extend device longevity. Despite promising short-term data, the long-term safety, tolerability, and efficacy of aDBS administered at home remain unclear, representing an unmet clinical need to guide therapeutic decisions in PD management.
Study Design
This international, prospective, open-label pivotal trial enrolled 68 PD participants between December 2020 and July 2022 across the United States, Canada, and Europe. Participants were selected if they were clinically stable on cDBS and medication regimens.
Following baseline assessments on cDBS, participants who tolerated both single-threshold and dual-threshold aDBS modes were randomized into a single-blind crossover phase, receiving each mode for 30 days with stable medication use. Those tolerating only one mode continued in that mode only. Subsequently, participants had the option to continue their preferred aDBS mode for an additional long-term follow-up lasting up to 10 months. Missing data for primary and secondary outcomes were addressed via multiple imputation techniques.
The two primary intervention modes utilized an embedded closed-loop stimulation system: single threshold aDBS (ST-aDBS) and dual threshold aDBS (DT-aDBS). The main comparator was the participants’ prior cDBS settings.
Main Outcomes and Measures
The primary endpoint targeted clinical efficacy, defined as at least 50% of participants achieving increased on-time without troublesome dyskinesias during aDBS compared to cDBS. On-time represented periods of satisfactory symptom control, documented via participant motor diaries. The threshold for meaningful improvement was set at no less than a 1-standard deviation reduction (post hoc defined as less than 2 hours per day reduction in on-time).
Secondary endpoints included total electrical energy delivered (TEED) as a measure of stimulation efficiency and battery longevity potential. Safety assessments systematically recorded adverse events (AEs), serious adverse events (SAEs), stimulation-related AEs, and device-related complications across the study duration.
Key Findings
Among 68 participants (mean age 62.2 years [SD 8.4]; 70.6% male), 40 received DT-aDBS and 35 received ST-aDBS during the crossover phase.
Both modes exceeded the primary endpoint performance goal: 91% of the DT-aDBS group and 79% of the ST-aDBS group met criteria for on-time improvement without troublesome dyskinesia, with no statistically significant difference between modes (χ2(1) = 1.0; P = 0.51).
TEED analysis showed a significant 15% mean reduction during ST-aDBS compared to cDBS (nominal P = 0.01), while DT-aDBS TEED was comparable to cDBS. This suggests energy efficiency improvements, particularly in ST-aDBS.
Safety profiles were favorable; all but one stimulation-related adverse event resolved during the initial aDBS configuration period. No serious device-associated adverse events occurred during long-term follow-up, underscoring the tolerability and safety of at-home aDBS therapy.
Exploratory analyses indicated that DT-aDBS may confer additional benefits by further increasing on-time without troublesome dyskinesias compared to cDBS, although larger confirmatory studies are warranted.
Expert Commentary
This study represents a landmark evaluation of personalized long-term aDBS treatment in PD, moving beyond controlled laboratory settings into patient homes. The high adherence and efficacy seen with both single and dual threshold modes validate the concept that closed-loop neuromodulation can adapt to fluctuating pathophysiology in PD, optimizing therapeutic windows.
The ability to reduce electrical energy delivery without compromising efficacy is clinically meaningful, as it may prolong device battery life and reduce replacement surgeries. Moreover, the near absence of serious adverse events demonstrates the safety of this advanced neuromodulation approach.
Limitations include the open-label design and relatively small sample size, which may underscore the need for larger randomized controlled trials to confirm long-term benefits and assess impacts on quality of life and healthcare utilization. The inclusion of mainly stable cDBS patients may also limit generalizability to newly implanted or more variable symptom populations.
Mechanistically, these findings emphasize that neural feedback-guided stimulation can dynamically target pathological oscillations associated with motor symptoms, harnessing technology to refine personalized neuromodulation.
Conclusion
This international pivotal trial establishes that long-term, at-home adaptive deep brain stimulation is a safe, effective, and tolerable treatment option for people with Parkinson’s disease stable on continuous DBS. Both single and dual threshold aDBS modes improve symptom-controlled on-time without increasing troublesome dyskinesias, with potential advantages in reducing electrical energy consumption.
These results open pathways for broader clinical adoption of personalized closed-loop DBS. Future research focusing on diverse PD populations, quality-of-life outcomes, and health economics will further inform integration into routine clinical practice.
References
Bronte-Stewart HM, Beudel M, Ostrem JL, et al; ADAPT-PD Investigators. Long-Term Personalized Adaptive Deep Brain Stimulation in Parkinson Disease: A Nonrandomized Clinical Trial. JAMA Neurol. 2025 Sep 22:e252781. doi:10.1001/jamaneurol.2025.2781 IF: 21.3 Q1 . Epub ahead of print. PMID: 40982287 IF: 21.3 Q1 ; PMCID: PMC12455485 IF: 21.3 Q1 .
Kuhn AA, Kempf F, Brucke C, et al. High-frequency stimulation of the subthalamic nucleus suppresses oscillatory beta activity in patients with Parkinson’s disease in parallel with improvement in motor performance. J Neurosci. 2008;28(24):6165-6173.
Little S, Pogosyan A, Neal S, et al. Adaptive deep brain stimulation in advanced Parkinson disease. Ann Neurol. 2013;74(3):449-457.
Herrington TM, Cheng JJ, Eskandar EN. Mechanisms of deep brain stimulation. J Neurophysiol. 2016;115(1):19-38.




I truly appreciate this post. I have been looking everywhere for this! Thank goodness I found it on Bing. You have made my day! Thank you again
Wonderful work! This is the type of information that should be shared around the net. Shame on Google for not positioning this post higher! Come on over and visit my website . Thanks =)