Highlights
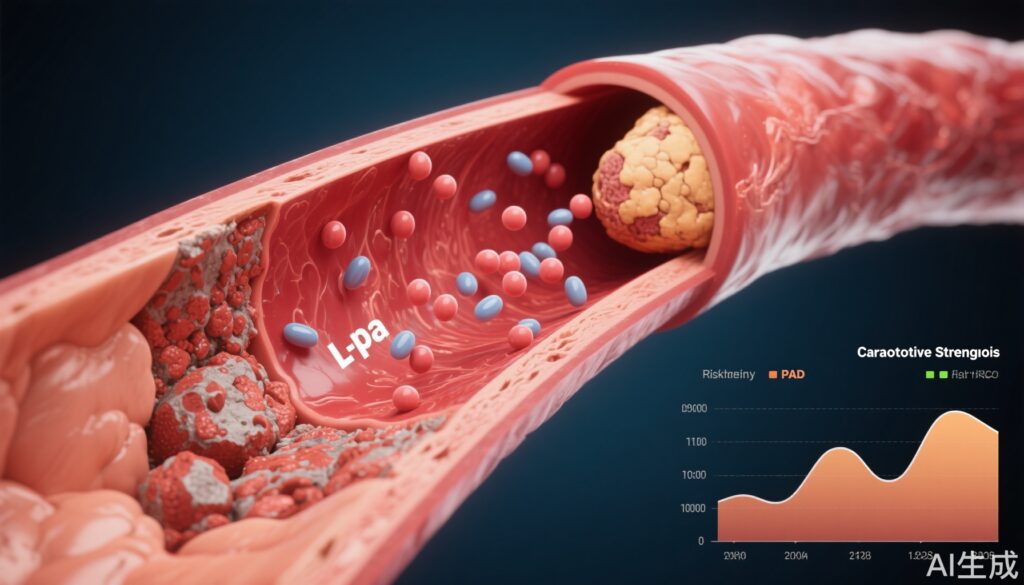
- Elevated lipoprotein(a) [Lp(a)] is a robust independent predictor for both incident and progressive peripheral artery disease (PAD) and carotid stenosis.
- Risk associations remain significant across diverse ethnicities and are independent of traditional risk factors such as hypertension, diabetes, and statin use.
- Reducing Lp(a) by 75 nmol/L could potentially decrease PAD risk by 20% and carotid stenosis risk by 16%.
Clinical Background and Disease Burden
Peripheral artery disease (PAD) and carotid artery stenosis are major contributors to global morbidity and mortality, representing advanced forms of atherosclerotic vascular disease outside the coronary circulation. Despite established risk factors—such as smoking, hypertension, diabetes, and dyslipidemia—there remains a significant proportion of residual vascular risk unexplained by conventional markers. Lipoprotein(a) [Lp(a)], a genetically determined, oxidized phospholipid-rich lipoprotein particle, has emerged as an independent causal risk factor for atherosclerosis, but its prognostic role in non-coronary vascular beds has historically lacked robust population-level evidence.
Research Methodology
This pivotal study, published in Circulation (Bellomo TR et al., 2025), leverages the UK Biobank, a large-scale, prospective cohort comprising 460,544 participants aged 40–69 at enrollment. Baseline data included comprehensive clinical profiles, Lp(a) levels measured by immunoturbidimetry (Denka Seiken method), and longitudinal electronic health records. PAD, carotid stenosis, and their progression events (major adverse limb events [MALE] and ischemic stroke) were rigorously defined using ICD-9/10 codes, UK procedural codes, and prescription records, ensuring high clinical fidelity. The study used Cox proportional hazards models to assess the association between incrementally increasing Lp(a) (per 75 nmol/L) and vascular event risk, adjusting for age, sex, genetic background, and major comorbidities. Sensitivity analyses included subgroup assessments by ethnicity, statin usage, BMI, and smoking status.
Key Findings
1. Lp(a) and Initial Disease Risk
- General population median Lp(a): 19.5 nmol/L.
- Incident PAD median Lp(a): 25.3 nmol/L; MALE progression: 33.3 nmol/L.
- Carotid stenosis median Lp(a): 29.5 nmol/L; ischemic stroke progression: 37.8 nmol/L.
- Each 75 nmol/L increase in Lp(a) was associated with an 18% higher risk of incident PAD (HR=1.18, 95% CI 1.15–1.20, P<0.0001) and a 17% higher risk of carotid stenosis (HR=1.17, 95% CI 1.13–1.20, P<0.0001).
2. Lp(a) and Disease Progression
- PATIENTS with baseline PAD and Lp(a) ≥150 nmol/L had a 57% increased risk of MALE (HR=1.57, 95% CI 1.14–2.16, P=0.006).
- For carotid stenosis, high Lp(a) was associated with a non-significant 40% increased risk of ischemic stroke (HR=1.40, 95% CI 0.81–2.40, P=0.228).
- Risk associations were consistent across age, sex, and genetic backgrounds, with no significant interactions detected.
3. Ethnic Variation and Risk Thresholds
- Marked differences in Lp(a) medians were observed across ethnic groups, but the risk relationship with PAD and carotid stenosis remained robust and consistent, supporting the use of universal Lp(a) risk thresholds.
- Reducing Lp(a) by 75 nmol/L is projected to lower PAD risk by 20% and carotid stenosis risk by 16%.
4. Interactions with Other Clinical States
- The Lp(a)-PAD risk association was amplified in patients who were statin-naïve, non-obese, or current smokers (interaction P-values: 0.003, 0.017, 0.014, respectively).
- Traditional risk factors (hypertension, diabetes, coronary artery disease, chronic kidney disease) did not materially modify the Lp(a)-PAD association.
Mechanistic Insights
The pathobiology of Lp(a) in atherogenesis is multifaceted. Lp(a) carries oxidized phospholipids that promote endothelial dysfunction, inflammation, and plaque instability. Its structural similarity to plasminogen may also impair fibrinolysis, further increasing thrombotic risk in the peripheral and carotid vasculature. The stability of Lp(a) levels across the lifespan and its resistance to conventional lipid-lowering therapies underscore its unique contribution to residual vascular risk.
Expert Commentary
Current clinical guidelines recognize Lp(a) as a risk enhancer but do not universally recommend routine screening outside high-risk or familial cases. This study provides compelling evidence for integrating Lp(a) measurement into broader risk stratification models for PAD and carotid stenosis, especially as Lp(a)-targeted therapies are advancing in clinical development.
Controversies and Limitations
While the UK Biobank offers unparalleled scale and phenotyping accuracy, findings may be limited by population selection bias and the lack of direct mechanistic or interventional data. The non-significant association with ischemic stroke in carotid stenosis patients likely reflects event rate limitations rather than a true absence of effect. Additionally, while the Denka Seiken assay is standardized, Lp(a) measurement remains a technical challenge in routine practice due to isoform variability.
Conclusion
Elevated Lp(a) is a potent, independent marker of both incident and progressive PAD and carotid stenosis across diverse populations. These findings call for the inclusion of Lp(a) in vascular risk assessment and bolster the rationale for dedicated Lp(a)-lowering interventions to address residual atherosclerotic risk beyond current therapies.
References
1. Bellomo TR, Bramel EE, Lee J, Urbut S, Flores A, Yu Z, et al. Evaluation of Lipoprotein(a) as a Prognostic Marker of Extracoronary Atherosclerotic Vascular Disease Progression. Circulation. 2025;152:00–00. doi:10.1161/CIRCULATIONAHA.124.073579
2. Tsimikas S. A Test in Context: Lipoprotein(a): Diagnosis, Prognosis, Controversies, and Emerging Therapies. J Am Coll Cardiol. 2017;69(6):692-711.
3. Nordestgaard BG, Chapman MJ, Ray K, et al. Lipoprotein(a) as a cardiovascular risk factor: current status. Eur Heart J. 2010;31(23):2844-2853.