Highlight
- High tibial osteotomy (HTO) slows medial articular cartilage loss in patients with varus alignment and medial compartment knee osteoarthritis (OA), compared to nonsurgical management alone.
- HTO leads to greater improvements in knee pain and function, as measured by the KOOS (Knee injury and Osteoarthritis Outcome Score).
- Clinical benefits were observed at two years, with only a minority of patients requiring further surgical intervention.
- Findings support early intervention, especially in younger patients with varus malalignment and less severe OA.
Background
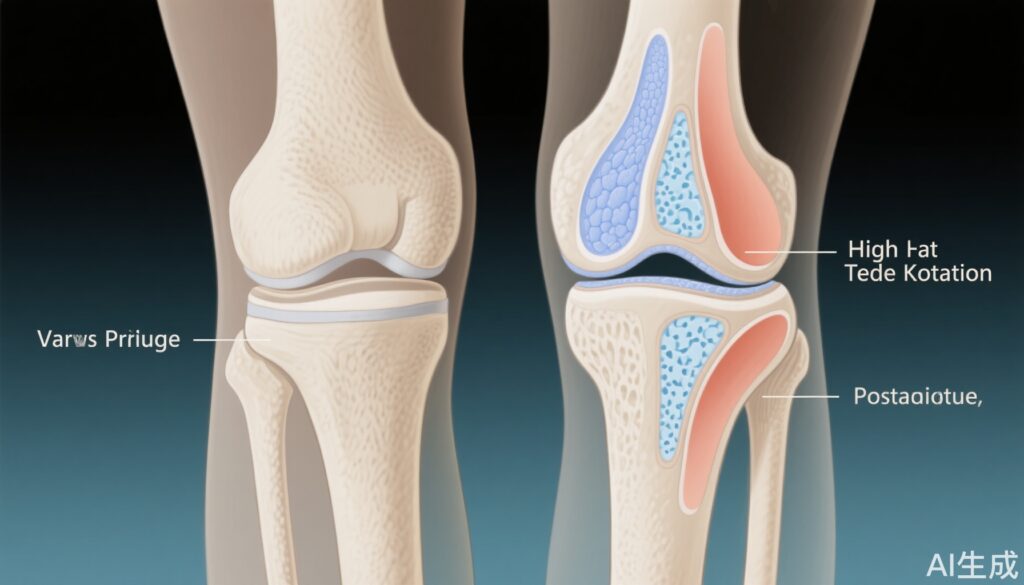
Knee osteoarthritis (OA) is a prevalent and disabling joint disorder, contributing significantly to pain, reduced mobility, and healthcare costs worldwide. Varus alignment, commonly known as bowlegs, is a recognized risk factor for both the onset and progression of medial compartment knee OA. The abnormal loading that results from varus alignment accelerates cartilage degeneration in the medial (inner) compartment. While total knee arthroplasty provides symptomatic relief for end-stage OA, there is a clinical need for joint-preserving interventions in younger, active adults.
High tibial osteotomy (HTO) is a surgical realignment procedure that shifts the mechanical axis from the overloaded medial compartment towards the lateral compartment, thereby reducing pathological stress and potentially slowing OA progression. Despite robust use in Europe and Asia, HTO remains relatively underutilized in North America, warranting high-quality evidence to define its role in contemporary practice.
Study Overview and Methodological Design
The recently published randomized controlled trial by Birmingham and colleagues (Ann Intern Med. 2025) provides critical data on the efficacy of HTO in this patient population. Conducted at the Fowler Kennedy Sport Medicine Clinic (London, Ontario), the study enrolled adults with radiographic medial compartment knee OA and varus alignment. Key eligibility criteria included symptomatic disease (average duration 7 years), a mean age in the mid-fifties, and BMI between 30-31 kg/m².
Participants were randomized to either HTO plus nonsurgical management or nonsurgical management alone. Nonsurgical management consisted of a structured 3-month exercise regimen (including in-person and home-based sessions) and ongoing nutritional counseling. A parallel preference arm allowed patients to select their preferred intervention, increasing real-world applicability. The primary endpoint was change in medial tibiofemoral articular cartilage thickness at two years, measured by advanced imaging. Secondary endpoints included KOOS and adverse event rates.
Key Findings
Among 124 patients completing two-year follow-up, those undergoing HTO experienced less medial cartilage loss (-0.07 mm, 2% loss from baseline) than controls (-0.25 mm, 9% loss), with a between-group difference of 0.18 mm. While the absolute difference did not reach the minimal clinically important difference (MCID, 6.3%), it represents a meaningful slowing of structural decline.
Clinically, total KOOS improved by 24.95 points in the HTO group versus 9.06 points in controls—a nearly 16-point difference, which exceeds commonly accepted thresholds for clinical significance. The parallel preference arm mirrored these results, bolstering the robustness of findings. Importantly, only five patients (across both arms) required additional surgery due to adverse events, indicating acceptable safety in a well-selected cohort.
Mechanistic Insights and Pathophysiological Context
Varus malalignment increases medial knee compartment load, accelerating cartilage degradation and OA progression. HTO alters the mechanical axis by creating an opening wedge in the proximal tibia, redistributing load more evenly across the knee. This biomechanical correction is hypothesized to decrease inflammatory and degenerative processes in the medial compartment, slowing structural and symptomatic deterioration. The observed improvements in KOOS and reduced cartilage loss align with this mechanistic rationale.
Clinical Implications
This trial affirms the disease-modifying potential of HTO for select patients with medial compartment OA and varus alignment, particularly those who are younger and have less advanced disease. Key takeaways for clinical practice include:
- Early consideration of HTO in active patients with symptomatic varus knee OA may delay or obviate the need for total knee arthroplasty.
- Comprehensive perioperative care, including exercise and nutrition counseling, is pivotal for optimizing outcomes.
- Patient selection remains critical—those with severe tricompartmental OA, advanced age, or significant comorbidities may derive less benefit.
Limitations and Controversies
Study limitations include a relatively short follow-up (2 years), modest sample size, and predominantly male, overweight cohort, which may limit generalizability. The cartilage thickness difference, while statistically significant, did not meet the MCID, warranting longer-term studies to confirm disease-modifying effects. Surgical expertise and post-operative protocols may vary across centers, potentially influencing outcomes. As HTO is less frequently performed in North America, broader adoption will require further surgeon training and patient education.
Expert Commentary or Guideline Positioning
Dr. S. Robert Rozbruch, a noted orthopedic surgeon not involved in the trial, emphasizes the principle that realignment preserves joint integrity and that HTO is most effective in younger patients with early OA. Current international guidelines recognize HTO as a viable option for unicompartmental OA with malalignment, but its uptake in North America lags behind other regions. Future guideline updates may increasingly reflect the accumulating evidence for HTO in this subgroup.
Conclusion
High tibial osteotomy, when combined with structured nonsurgical management, offers meaningful clinical and structural benefits for middle-aged adults with varus alignment and medial knee OA. The intervention slows cartilage loss, improves pain and function, and may defer the need for total knee replacement in appropriately selected patients. Ongoing research should focus on longer-term outcomes, optimization of patient selection, and strategies for broader implementation.
References
Birmingham TB, Primeau CA, Moyer RF, Bryant DM, Ma J, Leitch KM, Wirth W, Degen R, Getgood AM, Litchfield RB, Willits KR, Eckstein F, Giffin JR. High Tibial Osteotomy for Medial Compartment Knee Osteoarthritis: A Randomized Trial With Parallel Preference Arm. Ann Intern Med. 2025 Jul 29. doi: 10.7326/ANNALS-25-00920. Epub ahead of print. PMID: 40720836.
American Academy of Orthopaedic Surgeons. Treatment of Osteoarthritis of the Knee: Evidence-Based Guideline, 2nd Edition. 2013.
Felson DT, et al. Osteoarthritis: New Insights. Part 1: The Disease and Its Risk Factors. Ann Intern Med. 2000;133(8):635–646.