Highlight
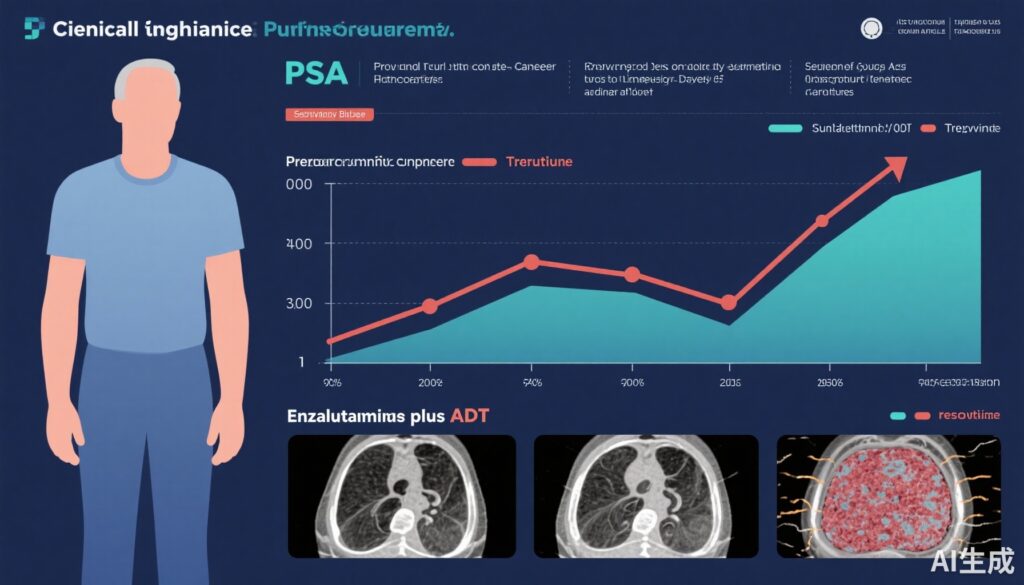
This secondary analysis of the ARCHES trial reveals that combining enzalutamide with androgen deprivation therapy (ADT) improves radiographic progression-free survival (rPFS) and overall survival (OS) in men with metastatic hormone-sensitive prostate cancer (mHSPC), regardless of baseline prostate-specific antigen (PSA) levels. Patients who achieved undetectable PSA (<0.2 ng/mL) during treatment experienced significantly reduced risks of radiographic disease progression and death, underscoring PSA decline as a robust surrogate marker of clinical outcome.
Study Background
Metastatic hormone-sensitive prostate cancer (mHSPC) represents an advanced disease state where prostate cancer has spread beyond the prostate but remains responsive to therapies that lower androgen levels. Androgen deprivation therapy (ADT) has been the cornerstone of treatment; however, resistance and progression remain key challenges. Prostate-specific antigen (PSA) is a biomarker widely used to monitor prostate cancer activity, and early PSA declines correlating with improved survival have been demonstrated in mHSPC patients. Enzalutamide, a potent androgen receptor inhibitor, has shown efficacy in metastatic castrate-resistant prostate cancer and more recently in hormone-sensitive settings when combined with ADT. Despite this, data delineating the relationship between PSA dynamics and clinical outcomes with enzalutamide plus ADT in mHSPC is limited, prompting this secondary analysis of the ARCHES trial.
Study Design
The ARCHES trial was a multinational, double-blind, phase 3 randomized clinical trial enrolling 1150 men with mHSPC between March 2016 and January 2018. Eligible patients were randomized 1:1 to receive either enzalutamide (160 mg daily) plus ADT or placebo plus ADT. Patients were allowed prior ADT for 3 to 6 months before enrollment. The primary endpoints included radiographic progression-free survival (rPFS) and overall survival (OS). This post hoc secondary analysis stratified patients by PSA levels at study entry, focusing on those with prior ADT exposure. PSA declines at 6 months, specifically achieving undetectable PSA (<0.2 ng/mL), were correlated with rPFS and OS outcomes. Follow-up periods included median durations of 14.4 months and 44.6 months for interim and final analyses, respectively.
Key Findings
Enzalutamide plus ADT significantly improved clinical outcomes compared to placebo plus ADT across various baseline PSA strata:
- In men with PSA ≤0.2 ng/mL, the hazard ratio (HR) for rPFS was 0.59 (95% CI, 0.27-1.30), indicating a trend toward benefit though not statistically definitive likely due to small subgroup size.
- For PSA between >0.2 and 4 ng/mL, rPFS was markedly improved with HR of 0.32 (95% CI, 0.20-0.50), a strong and statistically significant benefit.
- For PSA >4 ng/mL, rPFS also improved with HR 0.44 (95% CI, 0.32-0.62).
Critically, patients who achieved undetectable PSA during enzalutamide plus ADT therapy experienced:
- A striking 86% reduced risk of radiographic progression (HR, 0.14; 95% CI, 0.09-0.23; P < .001).
- A 76% reduction in mortality risk (HR, 0.24; 95% CI, 0.17-0.34; P < .001).
These data underscore the prognostic importance of PSA as both a predictive biomarker for response and a potential surrogate endpoint for long-term outcomes in mHSPC treatment.
Safety Considerations
While the focus of this secondary analysis was on efficacy endpoints and PSA dynamics, prior reports of the ARCHES trial have reported the safety profile of enzalutamide plus ADT as consistent with known effects, including fatigue, hypertension, and seizures in rare cases. No new safety signals emerged in these extended analyses.
Expert Commentary
The robust association between undetectable PSA and improved rPFS and OS observed in this subset analysis provides strong biological plausibility that deeper androgen receptor blockade yields durable clinical benefit. These findings align with prior evidence in prostate cancer demonstrating that the magnitude and rapidity of PSA suppression correlate with therapeutic success.
However, limitations include the post hoc nature of the analysis and variability in prior ADT exposure, which may affect PSA kinetics. Additionally, patients failing to achieve undetectable PSA despite enzalutamide plus ADT represent a high-risk subgroup that may benefit from therapeutic intensification or alternative approaches, warranting prospective validation.
Current guidelines increasingly recognize enzalutamide plus ADT as a standard of care in mHSPC, supported by data from multiple phase 3 trials including ARCHES. This analysis contributes valuable insight into PSA monitoring as a pragmatic and accessible tool to guide clinical decision-making, risk stratification, and patient counseling.
Conclusion
In men with metastatic hormone-sensitive prostate cancer, treatment with enzalutamide in combination with androgen deprivation therapy significantly improves clinical outcomes regardless of baseline PSA level. Achieving an undetectable PSA during therapy strongly predicts reduced disease progression and mortality, highlighting PSA decline as a meaningful surrogate marker. These findings emphasize the importance of early and deep PSA suppression in optimizing patient prognosis. Future studies should focus on strategies to further intensify treatment or switch therapies in patients who do not achieve undetectable PSA, improving personalized management of mHSPC.
Funding and Clinical Trials Registration
The ARCHES trial was funded by the pharmaceutical industry and oversight conducted according to ethical standards. Trial registration: ClinicalTrials.gov Identifier: NCT02677896.
References
Azad AA, Petrylak DP, Iguchi T, et al. Enzalutamide and Prostate-Specific Antigen Levels in Metastatic Prostate Cancer: A Secondary Analysis of the ARCHES Randomized Clinical Trial. JAMA Netw Open. 2025;8(5):e258751. doi:10.1001/jamanetworkopen.2025.8751.