Highlight
This nested substudy of the SCOT-HEART 2 trial evaluated the effect of coronary computed tomography (CT) angiography versus guideline-directed cardiovascular risk scoring on lifestyle behaviors, acceptance of preventive therapy, and cardiovascular risk factor modification. Compared with risk scoring, CT angiography led to higher adherence to healthy lifestyle components, greater acceptance of tailored preventive therapies, and small but meaningful reductions in 10-year cardiovascular risk, mainly in patients with CT-detected coronary atheroma.
Study Background and Disease Burden
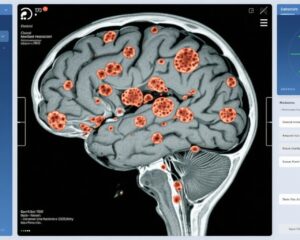
Cardiovascular disease (CVD) is a leading cause of global morbidity and mortality. Despite robust guideline recommendations emphasizing healthy lifestyle behaviors and primary preventive therapies (e.g., statins and antiplatelet agents), uptake remains suboptimal. Traditional cardiovascular risk scoring tools estimate individual risk primarily based on clinical and biochemical parameters but may lack personalized visualization of coronary artery disease burden. Coronary CT angiography offers direct anatomical visualization of coronary atherosclerosis and has potential to motivate patients toward improved behavior and acceptance of preventive therapies. However, the actual impact of CT angiography on lifestyle modification and preventive therapy uptake in asymptomatic, at-risk populations has not been widely established. This nested substudy within the SCOT-HEART 2 randomized clinical trial aimed to explore whether CT angiography could enhance adherence to preventive strategies beyond conventional risk scoring.
Study Design
This substudy was conducted from September 2020 to August 2024 within the framework of the SCOT-HEART 2 randomized clinical trial in Scotland. Participants were asymptomatic individuals aged 40 to 70 years, without known cardiovascular disease, and possessing at least one conventional cardiovascular risk factor. A total of 400 participants were enrolled and randomized to either cardiovascular risk scoring alone (n=195) or coronary CT angiography (n=205). Both groups received standardized lifestyle advice aimed at improving diet, smoking cessation, physical exercise, and body weight management.
Preventive therapy recommendations were guided by the respective diagnostic approach. In the risk-scoring arm, moderate-intensity statin therapy was advised for those with a 10-year cardiovascular risk ≥10%. In the CT angiography arm, recommendations included combined use of antiplatelet agents and moderate-intensity statins if coronary atherosclerosis was visualized, allowing a more personalized treatment approach.
The primary outcome measure was a composite of compliance with National Institute for Health and Care Excellence (NICE) guidelines concerning diet, body mass index (BMI), smoking status, and physical exercise at 6 months post-intervention. Secondary outcomes included acceptance rates of recommended preventive therapies, changes in lipid-lowering and antiplatelet therapy use, and quantified changes in cardiovascular risk factors and 10-year predicted risk.
Key Findings
Among the 400 participants enrolled, median age was 62 years (IQR 56-65), with 49.5% female, and a median predicted 10-year cardiovascular risk of 14% (IQR 9%-19%).
At 6 months, the CT angiography group showed a significantly higher rate of achieving the composite healthy lifestyle endpoint compared to risk scoring (17% vs 6%; odds ratio [OR] 3.42, 95% confidence interval [CI] 1.63-6.94; P < .001). This suggests that visualization of coronary atherosclerosis positively influenced lifestyle adherence.
Interestingly, fewer participants in the CT angiography group were recommended preventive therapy compared with the risk scoring group (51% vs 75%; P < .001). However, acceptance of prescribed therapies was substantially higher in the CT group (77% vs 46%; P < .001), resulting in comparable overall use of lipid-lowering agents (44% vs 35%; OR 1.43, 95% CI 0.96-2.15; P = .08). Additionally, antiplatelet therapy utilization was markedly higher in the CT angiography group (40% vs 0.5%; P < .001), reflecting the more tailored therapy based on imaging findings.
Improvements in cardiovascular risk factors and predicted 10-year risk were modest but more evident in those with CT-detected coronary atheroma, corroborating the potential of CT angiography to identify and target higher-risk individuals for intensified intervention.
Safety data and adverse events were not explicitly detailed in the substudy; however, the non-invasive nature of coronary CT angiography and the established safety profiles for statins and antiplatelets support the clinical applicability of these findings.
Expert Commentary
This substudy contributes valuable data supporting coronary CT angiography as an effective motivational and clinical tool in primary cardiovascular prevention. The marked increase in acceptance of preventive therapies after CT angiography likely stems from patients’ tangible visualization of atherosclerotic burden, which enhances perceived risk and justification for treatment. Furthermore, the reduction in over-prescription of preventive therapies compared to risk scoring may reflect more individualized risk stratification.
However, the absolute improvements in healthy lifestyle behaviors remain relatively modest, highlighting continued challenges in sustaining behavioral change. The study’s 6-month follow-up limits assessment of long-term adherence and cardiovascular outcomes. Additionally, results may be more applicable to populations with similar demographics and healthcare contexts.
Current guidelines emphasize risk-based preventive therapy; this study suggests that integrating imaging-based risk assessment could improve personalization and potentially uptake. Future large-scale studies are needed to confirm if these behavioral and therapeutic changes translate into significant reductions in cardiovascular events.
Conclusion
This nested substudy of the SCOT-HEART 2 trial demonstrates that coronary CT angiography, compared to traditional cardiovascular risk scoring, is associated with small but significant improvements in adherence to healthy lifestyle behaviors, higher acceptance rates of recommended preventive therapies, and modest risk factor modification in asymptomatic individuals at elevated cardiovascular risk. The approach enables more personalized preventive care and may refine risk stratification beyond conventional scoring methods. However, the clinical impact on hard cardiovascular endpoints remains to be determined. Clinicians should consider the potential motivational advantages of imaging in preventive cardiology while continuing to emphasize comprehensive lifestyle interventions.
References
- McDermott M, Khaing PH, Meah MN, et al. CT Angiography, Healthy Lifestyle Behaviors, and Preventive Therapy: A Nested Substudy of the SCOT-HEART 2 Randomized Clinical Trial. JAMA Cardiol. 2025;10(8):841-850. doi:10.1001/jamacardio.2025.1763
- National Institute for Health and Care Excellence. Cardiovascular disease: risk assessment and reduction, including lipid modification. NICE guideline [CG181]. 2016. Available at: https://www.nice.org.uk/guidance/cg181
- Williams MC, Newby DE, Dweck MR. Computed tomography coronary angiography: clinical advances and future directions. Nat Rev Cardiol. 2023;20(1):56-72. doi:10.1038/s41569-022-00735-z
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. Circulation. 2019;140(11):e596-e646. doi:10.1161/CIR.0000000000000678