Highlights
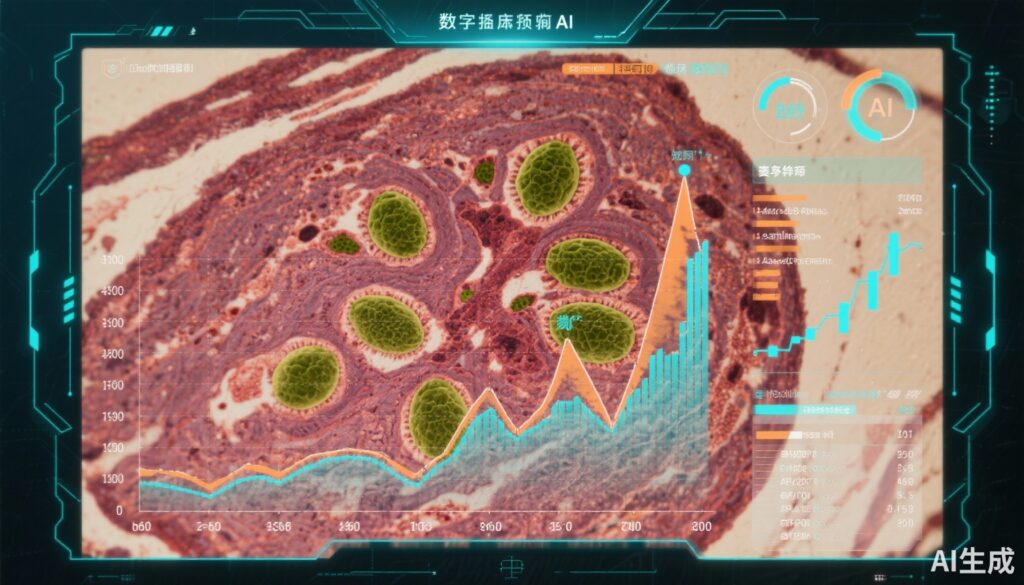
- First large-scale, multicenter cohort utilizing AI (Hover-NeXt) to quantify TILs on routine H&E slides in advanced melanoma.
- AI-detected TIL density robustly correlates with objective response rate, progression-free survival, and overall survival in patients receiving anti-PD-1-based therapies.
- AI scoring demonstrated stronger predictive accuracy than manual TIL assessments, suggesting superior reproducibility and clinical utility.
- Findings support clinical implementation of AI-assisted TIL quantification as an accessible, cost-effective biomarker for ICI response, with publicly available model resources to foster validation.
Background
Melanoma remains a significant clinical challenge due to its aggressive nature and propensity for metastasis. Immune checkpoint inhibitors (ICIs), specifically anti-PD-1 and combination anti-PD-1 plus anti-CTLA-4 therapies, have transformed advanced melanoma management, yet reliable, universally accessible predictive biomarkers are lacking. Tumor-infiltrating lymphocytes (TILs) reflect the host immune response within the tumor microenvironment and have been shown to be associated with ICI efficacy. However, traditional manual scoring of TILs is time-consuming, subjective, and prone to interobserver variability, limiting its routine clinical use. The advent of artificial intelligence (AI) offers powerful tools for standardized histopathological analysis, enabling objective and reproducible quantification of TILs from hematoxylin-eosin (H&E) stained slides.
Key Content
Chronological Development and Validation of AI-Based TIL Quantification
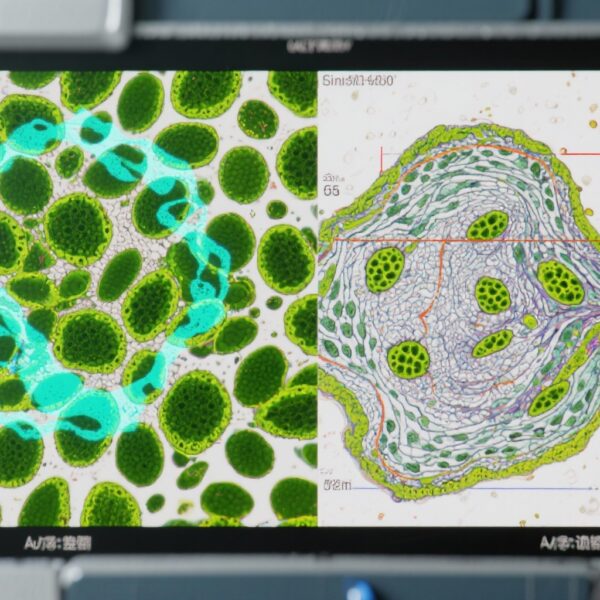
The landmark study by Schuiveling et al. (JAMA Oncol. 2025) conducted a multicenter cohort investigation involving 1202 patients with advanced cutaneous melanoma across 11 Dutch centers. Patients were treated with first-line anti-PD-1 therapy, either as monotherapy or combined with anti-CTLA-4. Utilizing the Hover-NeXt convolutional neural network—trained on an independent set with over 161,000 pathologist-verified cell annotations—the percentage of TILs within manually annotated tumor regions on pretreatment H&E slides was quantified.
The median TIL density was 9.9%, spanning from 0.3% to 69.4%. Statistical analyses adjusted for confounding clinical variables (age, sex, stage, ICI regimen, BRAF status, presence of brain metastases, lactate dehydrogenase levels, and performance status) demonstrated that every 10% increment in AI-detected TILs was associated with a significantly increased objective response rate (ORR, adjusted odds ratio 1.40; 95% CI, 1.23-1.59), prolonged progression-free survival (PFS, adjusted hazard ratio 0.85; 95% CI, 0.79-0.92), and improved overall survival (OS, adjusted hazard ratio 0.83; 95% CI, 0.76-0.91). Importantly, these associations were consistent across monotherapy and combination ICI cohorts.
Comparison to Manual TIL Scoring and Other Biomarker Modalities
Manual TIL counts following the Immuno-Oncology Biomarkers Working Group guidelines were also performed in this cohort. AI-based TIL quantification showed stronger correlations with clinical outcomes than manual assessments, illustrating improved sensitivity and objectivity. These findings mirror prior smaller studies highlighting tumor-infiltrating CD8+ T cell density as predictive for anti-PD-1 therapy effects in melanoma and non-small cell lung cancer (NSCLC), expanded here by an advanced algorithm capable of comprehensive, reproducible evaluation on standard H&E slides.
Additionally, complementary studies have established the role of CD8+/CD4+ TIL ratios and specific lymphocyte densities in predicting ICI response, underscoring the immunologic basis for TILs as biomarkers. Other exploratory avenues, including gut microbiome modulation and adoptive TIL transfer, further validate the centrality of immune infiltrates in modulating anti-tumor response.
Clinical Implications and Integration into Practice
The study advocates for adopting AI-assisted TIL quantification as a convenient biomarker in the pretherapeutic assessment of melanoma metastases. Given the universal availability of H&E-stained tumor tissue and the growing accessibility of computational pathology platforms, this approach offers a scalable, cost-effective solution compared to molecular assays or complex immunohistochemistry panels. Its predictive value for survival and response supports its use in treatment stratification, potentially guiding ICI choice or intensification.
Moreover, public sharing of the Hover-NeXt architecture and model weights promotes validation and widespread implementation, facilitating personalized immunotherapy strategies across institutions.
Expert Commentary
The integration of AI modalities into pathologic diagnostics represents a frontier in oncologic precision medicine. This comprehensive study exemplifies how AI can augment, and potentially surpass, traditional manual methods in biomarker detection. Notably, the robust adjustment for multiple prognostic confounders strengthens the validity of AI-detected TILs as an independent biomarker.
However, limitations include retrospective cohort design, potential selection biases, and reliance on available archival tissue. Prospective studies are warranted to confirm clinical utility in decision-making workflows, including predictive power across diverse melanoma subtypes and in non-cutaneous melanoma.
Biologically, elevated TIL densities likely denote pre-existing antitumor immunity poised for re-invigoration upon PD-1 blockade. The superior performance of AI likely stems from its capacity for consistent, large-scale cellular classification and spatial assessment, accounting for heterogeneous tumor microenvironments.
These findings align with complementary research on combined modalities, such as TIL adoptive immunotherapy and microbiota modulation, painting an integrated picture of immune engagement’s role in therapeutic efficacy.
Conclusion
Artificial intelligence-detected tumor-infiltrating lymphocytes on routine hematoxylin-eosin slides serve as a powerful, accessible biomarker predicting response and survival in advanced melanoma treated with anti-PD-1-based immunotherapy. The methodological rigor and scale of the reported study provide compelling evidence for clinical adoption, heralding a new era of AI-integrated pathology that enhances personalized treatment planning. Future directions include prospective validation across broader patient populations, integration with multi-omic and spatial profiling, and exploration of AI biomarkers in other tumor contexts to optimize immunotherapy outcomes.
References
- Schuiveling M, et al. Artificial Intelligence-Detected Tumor-Infiltrating Lymphocytes and Outcomes in Anti-PD-1-Based Treated Melanoma. JAMA Oncol. 2025 Oct 16:e254072. doi: 10.1001/jamaoncol.2025.4072. PMID: 41100131; PMCID: PMC12532025.
- van den Berg J, et al. The role of tumor-infiltrating lymphocytes as a predictive biomarker of response to anti-PD1 therapy in metastatic melanoma and NSCLC. Med Oncol. 2018 Jan;35(3):25. doi:10.1007/s12032-018-1080-0. PMID: 29388007.
- Riaz N, et al. Tumor and Microenvironment Evolution during Immunotherapy with Nivolumab. Cell. 2017;171(4):934-949.e16. doi:10.1016/j.cell.2017.09.028. PMID: 29056344.
- Davoli T, et al. Tumor aneuploidy correlates with markers of immune evasion and with reduced response to immunotherapy. Science. 2017;355(6322). doi:10.1126/science.aaf8399.