Study Background and Disease Burden
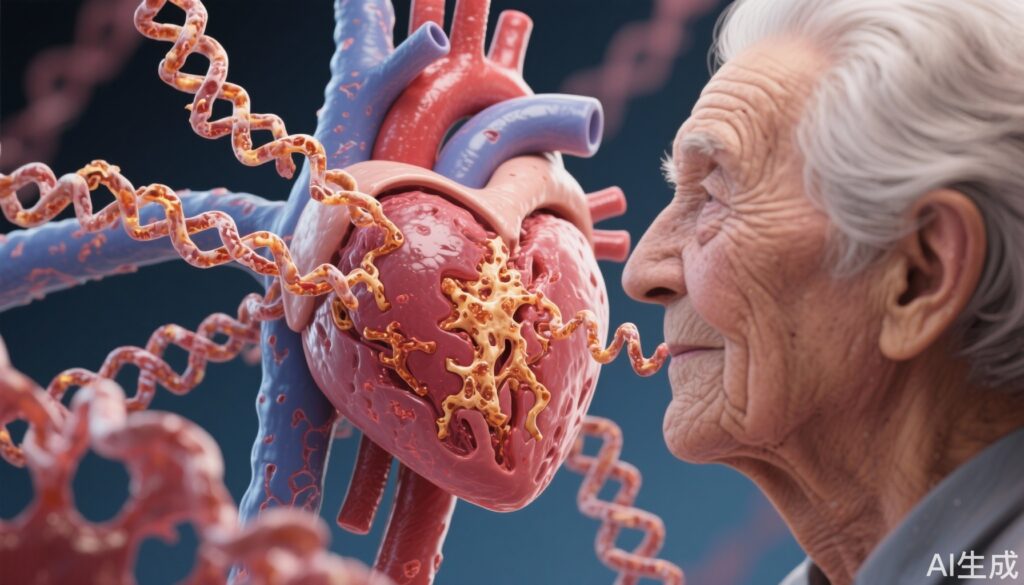
Advanced glycation end-products (AGEs) are proteins or lipids that become nonenzymatically glycated and oxidized after exposure to sugars and oxidative stress. This chemical modification is significantly increased under hyperglycemic conditions and with aging, processes common in the elderly population. AGEs, particularly Nε-carboxymethyl-lysine (CML), accumulate in tissues including the heart and vasculature, and contribute to alterations in structural and functional integrity. These changes potentially foster the pathogenesis of cardiovascular diseases such as heart failure (HF) and atrial fibrillation (AF), conditions that impose substantial morbidity and mortality burdens in older adults. Despite established mechanistic links, prospective epidemiological data on circulating AGEs and incident HF or AF risk in aging populations have been lacking, representing a critical knowledge gap in cardiovascular geriatric care and preventive cardiology.
Study Design
The Cardiovascular Health Study (CHS) is a prospective, population-based cohort study designed to investigate risk factors for cardiovascular disease and stroke in community-dwelling older adults. In this analysis, 2685 participants with mean age 77±5 years, 63% women, and 17% diabetics were included. Serum levels of Nε-carboxymethyl-lysine (CML), a principal AGE formed in tissue proteins, were quantified by immunoassay. Participants were followed for a median of 9 years for the development of incident heart failure and atrial fibrillation events. Secondary analyses evaluated incident HF subtypes (e.g., preserved vs reduced ejection fraction) and associations with baseline echocardiographic cardiac mechanics. Extensive adjustments were made to account for confounders and potential mediators, including renal function markers (estimated glomerular filtration rate and urine albumin-creatinine ratio), time-updated myocardial infarction events, and natriuretic peptide levels.
Key Findings
During follow-up, 832 incident HF and 1016 incident AF events were observed. After multivariable adjustment for demographic and clinical confounders, each standard deviation increment in serum CML was associated with a significantly increased risk of incident HF (hazard ratio [HR] 1.10, 95% confidence interval [CI] 1.02–1.17) and AF (HR 1.09, 95% CI 1.02–1.16). However, the AF association became non-significant after further adjustment for renal function parameters, namely estimated glomerular filtration rate and urine albumin-creatinine ratio, implying renal impairment may mediate this relation. Similarly, the CML–HF association was attenuated and lost statistical significance after incorporating time-updated myocardial infarction events as a covariate, suggesting that ischemic heart disease intermediates are important contributors to HF risk in the context of elevated CML.
Additionally, when analyses adjusted for natriuretic peptides (biomarkers indicating cardiac stress and heart failure risk) or excluded participants with elevated baseline natriuretic peptide levels, the associations between CML and both HF and AF were nullified. These findings imply that advanced cardiac remodeling or subclinical cardiac dysfunction may lie on the causal pathway between AGEs and overt HF/AF.
Secondary analyses investigating HF subtypes—either heart failure with preserved ejection fraction (HFpEF) or reduced ejection fraction (HFrEF)—and key echocardiographic parameters of cardiac mechanics showed no statistically significant independent associations with serum CML levels. This suggests that the serum CML effects observed may not directly translate to specific HF phenotypes or measurable baseline cardiac mechanical dysfunction but potentially reflect a broader systemic pathological process.
Expert Commentary
This prospective study contributes critical epidemiological evidence that serum CML—a measurable circulating advanced glycation end-product—is associated with increased incidence of heart failure and atrial fibrillation in a well-characterized cohort of older adults. The findings align with in vitro and animal model data implicating AGE-mediated cross-linking and inflammation in cardiovascular tissue remodeling. Notably, the attenuation of risk after adjustment for myocardial infarction and renal function markers indicates a complex interplay between AGE accumulation, ischemic injury, and renal impairment in promoting cardiac morbidity.
These observations raise the possibility that therapeutic strategies targeting AGE accumulation or its downstream signaling pathways—such as AGE cross-link breakers, receptor for AGE (RAGE) antagonists, or antioxidant therapies—could be beneficial in preventing HF and AF, especially in vulnerable aged populations. However, due to the observational nature of the study, causality cannot be definitively established. Moreover, the lack of association with cardiac mechanics suggests circulating CML may serve more as a systemic biomarker of risk rather than a direct mediator of specific myocardial dysfunction.
It is also critical to recognize that the study population consisted of older adults predominantly without advanced baseline cardiac dysfunction, and whether these results generalize to younger populations or those with established cardiovascular disease requires further investigation. Future studies should also elucidate mechanisms by which kidney function mediates AGE-related cardiac risks.
Conclusion
In summary, serum Nε-carboxymethyl-lysine, a major circulating advanced glycation end-product, is prospectively associated with incident heart failure and atrial fibrillation risk in older adults, independent of conventional risk factors. This relationship appears partially mediated through myocardial infarction and renal function alterations and may be influenced by underlying subclinical cardiac stress. These findings underscore the potential clinical value of AGEs as biomarkers and therapeutic targets to mitigate HF and AF incidence in the aging population. Continued research into AGE-related cardiovascular pathobiology and intervention studies of AGE-modulating therapies are warranted to improve prevention and management strategies for geriatric cardiology patients.
References
1. Bene-Alhasan Y, Bartz TM, Djoussé L, et al. Advanced Glycation End-Product Carboxymethyl-Lysine and Incident Heart Failure and Atrial Fibrillation in Older Adults. J Am Heart Assoc. 2025 Sep 5:e040640. doi:10.1161/JAHA.124.040640. Epub ahead of print. PMID: 40913281.
2. Semba RD, Ferrucci L, Sun K, et al. Advanced glycation end products and their circulating receptors predict cardiovascular disease mortality in older community-dwelling women. Aging Clin Exp Res. 2009;21(5-6):182-190.
3. Vlassara H, Palace MR. Diabetes and advanced glycation endproducts. J Intern Med. 2002;251(2):87-101.
4. Ramasamy R, Vannucci SJ, Yan SS, et al. Advanced glycation end products and RAGE: a common thread in aging, diabetes, neurodegeneration, and inflammation. Glycobiology. 2005 Jul;15(7):16R-28R.
5. Chrysohoou C, Tousoulis D, Antoniades C, et al. Oxidative stress and endothelial dysfunction in heart failure. Heart Fail Rev. 2009 Jan;14(1):83-91.