Highlight
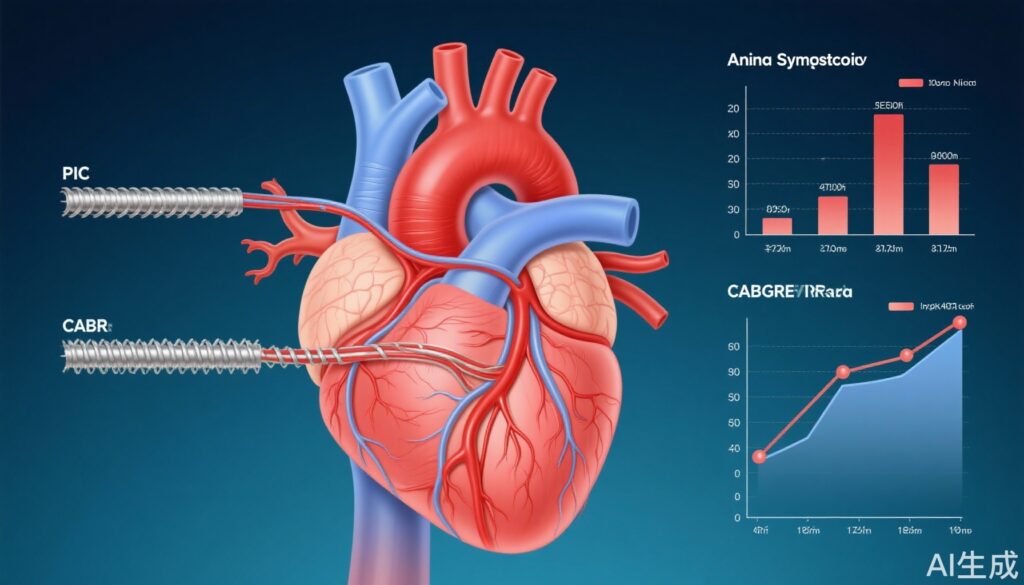
- Both percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) improve health status in chronic coronary disease (CCD) versus conservative management, according to ISCHEMIA.
- CABG provides greater angina relief than PCI at 1 year post-procedure but these differences equalize by 3 years.
- Health status improvements were measured by the Seattle Angina Questionnaire (SAQ) scores, offering patient-centered evidence for treatment selection in CCD.
Study Background and Disease Burden
Chronic coronary disease (CCD) represents a significant global health burden due to its high prevalence, morbidity, and impact on quality of life, primarily attributable to angina and ischemia. Management strategies include conservative medical therapy and invasive procedures such as PCI and CABG. While the ISCHEMIA trial established that an invasive strategy improves health status outcomes compared to conservative management, questions remained whether these benefits stem predominantly from CABG, which has historically been reported to offer superior symptomatic relief compared to PCI. Understanding how PCI and CABG differentially affect patient-reported outcomes over time is critical for personalized treatment decisions in CCD.
Study Design
This comparative analysis was conducted within the framework of the international multicenter ISCHEMIA trial (NCT01471522). Participants with moderate or severe ischemia and chronic coronary disease were assigned either to a conservative strategy (n=2232) or invasive management. The invasively managed cohort was subdivided into patients treated with PCI (n=1198) or CABG (n=340) based on clinical indications and multidisciplinary decisions. The primary outcomes were health status measures evaluated by the Seattle Angina Questionnaire-7 summary score (SAQ-SS) and angina frequency score (SAQ-AF), with higher scores denoting better health status and lower angina frequency. Proportional odds models adjusted for demographic, clinical, and angiographic variables were utilized to compare the 1- and 3-year outcomes across groups.
Key Findings
Patients in all three groups experienced improvement in health status over baseline. At 1 year, SAQ-SS increased by 9.9 ± 18.1 points in the conservative group, 15.7 ± 19.3 points in the PCI group, and 16.1 ± 19.1 points in the CABG group. By 3 years, the improvements persisted with increases of 11.5 ± 20.2, 16.5 ± 21.8, and 15.0 ± 19.4 points, respectively. Freedom from angina at 1 year was highest in the CABG group (82.4%), followed by PCI (73.3%), and lowest in the conservative group (61.4%). Similar trends were sustained at 3 years (CABG 81.4%, PCI 76.1%, conservative 70.4%).
Risk-adjusted analyses demonstrated that both PCI and CABG were significantly associated with higher SAQ-SS and SAQ-AF scores compared to conservative management at both 1 and 3 years. Notably, CABG showed a significantly higher odds of angina freedom compared to PCI at 1 year (odds ratio 1.54; 95% CI, 1.03–2.31). However, at 3 years, no significant differences were observed between CABG and PCI, either in SAQ-SS (odds ratio 1.11; 95% CI, 0.78–1.57) or SAQ-AF (odds ratio 0.94; 95% CI, 0.58–1.54).
These findings suggest that while CABG may provide greater early angina relief, the long-term health status benefits of PCI and CABG converge, reinforcing the role of both revascularization strategies in selected patients with CCD.
Expert Commentary
The ISCHEMIA trial’s substudy delivers meaningful patient-centered data that complement traditional endpoints such as mortality and myocardial infarction. The early advantage of CABG in angina relief may be attributable to the more complete revascularization achieved by bypass surgery, particularly in multivessel disease. Nonetheless, by 3 years, the symptomatic benefits balance out, possibly due to improvements in PCI techniques and medical therapies.
While the trial adjusts for many confounders, some limitations include the inherent selection bias in assigning PCI versus CABG and the relatively smaller CABG sample size. Moreover, patient preferences, anatomical complexity, and procedural risks must be integrated into treatment decisions. These results underscore the need for individualized decision-making integrating health status outcomes, anatomy, comorbidities, and patient values.
Guidelines have increasingly incorporated health status measures to guide revascularization decisions, and these findings support a nuanced approach where both PCI and CABG are valid options for symptom relief, with CABG offering an early advantage that may diminish over time.
Conclusion
In patients with chronic coronary disease and moderate to severe ischemia, both PCI and CABG significantly enhance health status outcomes compared to conservative management, with sustained improvements up to 3 years. CABG provides superior angina relief compared to PCI at 1 year, but this benefit is not sustained at 3 years. These data emphasize that both invasive strategies remain central to symptom management in CCD, and procedural choice should be personalized based on clinical, anatomical, and patient-centered factors.
References
1. Huded CP, Spertus JA, Jones PG, O’Brien SM, Mark DB, Bangalore S, Stone GW, Williams DO, White HD, Boden WE, Reynolds HR, Hochman JS, Maron DJ; ISCHEMIA Research Group. Health Status Outcomes With Percutaneous Coronary Intervention and Coronary Artery Bypass Grafting in ISCHEMIA. Circulation. 2025 Sep 5. doi: 10.1161/CIRCULATIONAHA.125.073591. Epub ahead of print. PMID: 40910165.
2. Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O’Brien SM, Boden WE, et al.; ISCHEMIA Research Group. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N Engl J Med. 2020;382:1395–1407.
3. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407-477.