Study Background and Disease Burden
Coronary artery disease (CAD) remains a leading cause of morbidity and mortality worldwide, underscoring the critical need for effective secondary prevention strategies. Aspirin has long been established as a cornerstone in reducing recurrent cardiovascular events by inhibiting platelet aggregation. Clinical guidelines widely recommend aspirin monotherapy to prevent secondary cardiovascular events in patients with established CAD. However, these recommendations have largely been based on earlier trials with limited follow-up durations, modest sample sizes, and without head-to-head comparisons against newer antiplatelet agents over extended timeframes.
Recent advances have introduced P2Y12 receptor inhibitors such as clopidogrel, known to exert antithrombotic effects through a distinct mechanism, prompting re-examination of the relative efficacy and safety profiles of these agents. This has particular importance given the potential for improved outcomes and individualized treatment approaches in diverse patient populations, including those with genetic polymorphisms affecting drug metabolism.
Study Design
The recently published meta-analysis in The Lancet by Valgimigli et al. represents the most comprehensive assessment to date comparing clopidogrel with aspirin for secondary prevention in CAD. Researchers systematically retrieved and synthesized data from seven randomized clinical trials (ASCET, CADET, CAPRIE, HOST-EXAM, STOPDAPT-2, STOPDAPT-3, and SMART-CHOICE-3) enrolling a total of 28,982 patients. Among them, 14,507 patients received clopidogrel and 14,475 received aspirin. The included studies featured heterogeneous CAD populations, many having undergone percutaneous coronary intervention (PCI) or presenting with acute coronary syndromes, and most patients had discontinued or not received dual antiplatelet therapy at baseline.
The primary efficacy endpoint was the occurrence of major adverse cardiovascular and cerebrovascular events (MACCE), a composite of cardiovascular death, myocardial infarction, or stroke. The primary safety endpoint was major bleeding, defined primarily as BARC type 3 or 5 bleeding events. Median follow-up across trials was 2.3 years, with the maximum follow-up extending to 5.5 years.
Key Findings
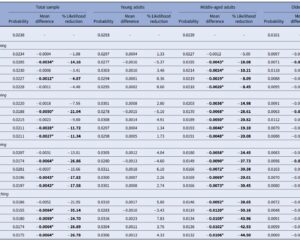
The meta-analysis demonstrated that clopidogrel was superior to aspirin in preventing MACCE. Specifically, the incidence rate of MACCE was 2.61 per 100 patient-years in the clopidogrel group versus 2.99 per 100 patient-years in the aspirin group, yielding a hazard ratio of 0.86 (95% CI, indicating a 14% relative risk reduction). Importantly, this benefit was maintained over the longest follow-up period of 5.5 years.
Regarding safety, the incidence of major bleeding events did not differ significantly between groups, suggesting that clopidogrel’s enhanced efficacy did not come at the cost of increased bleeding risk. Additionally, clopidogrel led to a 11% relative risk reduction in net adverse cardiovascular and cerebrovascular events (NACE), encompassing ischemic and bleeding outcomes (risk ratio 0.89).
Subgroup analyses enriched the findings, revealing that even patients harboring CYP2C19 loss-of-function polymorphisms—known to impair clopidogrel metabolism—experienced superior secondary prevention than with aspirin. This is particularly informative given that approximately two-thirds of participants were East Asian, a population with a high prevalence of such genetic variants.
Notably, the inclusion of head-to-head clinical trials such as STOPDAPT-3 and SMART-CHOICE-3 provided compelling contemporary evidence to challenge the predominant aspirin-centered paradigm.
Mechanistic Insights
Aspirin inhibits cyclooxygenase-1 (COX-1), reducing thromboxane A2 synthesis and thereby decreasing platelet aggregation. In contrast, clopidogrel selectively and irreversibly blocks the P2Y12 receptor on platelet surfaces, preventing adenosine diphosphate (ADP)-mediated platelet activation and aggregation. These distinct but complementary pathways explain the rationale for dual antiplatelet therapy (DAPT) in high-risk subsets.
Given this mechanistic distinction, clopidogrel monotherapy may offer more potent inhibition of platelet activation relevant to atherothrombotic events in CAD, resulting in the observed reduction in MACCE without a corresponding increase in bleeding.
Expert Commentary
This landmark meta-analysis represents a paradigm shift in secondary prevention for CAD. While aspirin has been a mainstay, the extensive and rigorous data now favor clopidogrel as the preferred monotherapy, especially for long-term management beyond the conventional 2-4 years previously studied. The broad inclusion criteria and diverse populations enhance the applicability of these findings globally.
Clinicians should be reassured by the maintained safety profile of clopidogrel, alongside its superior efficacy. The findings also prompt reconsideration in clinical guidelines, potentially advocating clopidogrel over aspirin for long-term secondary prevention in most patients.
Limitations include inherent heterogeneity among trials and populations. The genetic aspect, although addressed, warrants further personalized medicine approaches. Future research should explore direct comparisons with newer P2Y12 inhibitors and evaluate cost-effectiveness in various healthcare settings.
Conclusion
In summary, this comprehensive individual patient data meta-analysis unequivocally demonstrates that clopidogrel provides superior secondary prevention of cardiovascular events compared to aspirin in patients with CAD over a long-term follow-up of up to 5.5 years without added bleeding risk. These findings support a shift in clinical practice toward favoring clopidogrel monotherapy for CAD secondary prevention. Clinicians and guideline committees should integrate this robust evidence to optimize cardiovascular risk management in diverse populations, including those with genetic variants impacting drug metabolism.
References
[1] Valgimigli, M., Choi, K. H., Giacoppo, D., et al. (2025). Clopidogrel versus aspirin for secondary prevention of coronary artery disease: A systematic review and individual patient data meta-analysis. The Lancet. Advance online publication. https://doi.org/10.1016/S0140-6736(25)01562-4