Study background and disease burden
Fasting-mimicking diets (FMDs) have garnered increasing attention as nutritional interventions that replicate the physiological benefits of fasting while providing minimal caloric intake. These diets demonstrate promise in improving cardiometabolic health parameters and stimulating autophagy, a cellular recycling process critically implicated in ageing and metabolic regulation. Most clinical research has predominantly targeted low-protein FMDs to enhance autophagic responses and reduce ageing-related risk factors. However, macronutrient composition beyond caloric restriction may crucially influence the spectrum of metabolic adaptations, including lipid metabolism, cardiovascular function, and microbiome dynamics. Cardiometabolic disease remains a leading cause of morbidity worldwide, driving the need for effective, tolerable dietary interventions. Investigating how protein content within FMDs affects health outcomes addresses an unmet clinical need to tailor personalized nutrition strategies for cardiometabolic risk reduction and healthy ageing.
Study design
Burns et al. conducted a prospective, randomized, parallel group clinical trial involving 46 healthy adult participants. The cohort included both men and women with an average age ranging from 35 to 41 years and a body mass index (BMI) within normal limits to overweight. Participants were randomly assigned into three groups: a control group maintained on an isoenergetic diet (n=16), a low-protein/high-fat fasting-mimicking diet (LP-FMD; 850 kcal/day with 10% protein and 45% fat; n=15), and a high-protein/low-fat fasting-mimicking diet (HP-FMD; 850 kcal/day with 30% protein and 25% fat; n=15). The intervention spanned seven days.
Comprehensive assessments included blood and fecal sample collection to analyze metabolic, inflammatory, and microbiome markers, body composition evaluation using dual-energy X-ray absorptiometry (DEXA) scanning, and cardiovascular function tests including heart rate variability measures, all conducted before and after the intervention period. The study was registered under ClinicalTrials.gov (Identifier NCT06560996). This design allowed for comparative analyses of macronutrient composition effects on multiple physiological, metabolic, and molecular endpoints associated with cardiometabolic health and autophagy.
Key findings
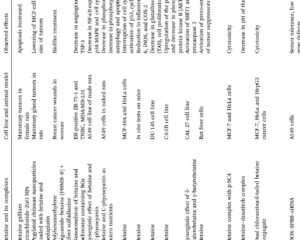
Both fasting-mimicking diets induced significant reductions in body weight and overall fat mass (interaction P < 0.0001) compared to the control group. However, unique effects were observed between the LP-FMD and HP-FMD groups. Visceral fat mass, a key cardiometabolic risk factor, was reduced significantly only in the HP-FMD group relative to control (mean difference: -0.09 kg; 95% CI: -0.15 to -0.03; P = 0.006). This finding underscores the potential selective benefit of higher protein intake combined with lower fat content in targeting metabolically detrimental fat depots.
Both FMD protocols decreased fasting plasma glucose levels by approximately 10%, with reductions measured as -0.41 mmol/L (95% CI: -0.80 to -0.02; P = 0.038) for LP-FMD and -0.46 mmol/L (95% CI: -0.74 to -0.17; P = 0.003) for HP-FMD. Concurrently, serum insulin-like growth factor 1 (IGF1) dropped by around 35% in both groups relative to control (LP-FMD: -9.0 nmol/L, P < 0.0001; HP-FMD: -5.4 nmol/L, P = 0.024), indicating consistent modulation of anabolic signaling pathways implicated in ageing and metabolic disease.
The LP-FMD group exhibited a significantly greater increase in serum hydroxybutyrate (a ketone body linked to metabolic adaptation during fasting) than the HP-FMD group (mean difference 0.64 mmol/L; 95% CI: 0.13 to 1.15; P = 0.015). This difference likely reflects enhanced ketogenesis in response to higher fat intake and lower protein availability.
Notably, HP-FMD uniquely improved heart rate variability (P < 0.0001), a non-invasive biomarker of autonomic cardiovascular regulation and resilience. Concomitantly, gut microbiome diversity increased significantly (P = 0.003), alongside favorable shifts in circulating lipid profiles—specifically lowering triglycerides (P = 0.009) and saturated fatty acids (P = 0.008)—highlighting the pleiotropic benefits of this macronutrient pattern.
At the molecular level, both diets stimulated autophagy-related pathways, supporting their mechanistic role in promoting cellular homeostasis and mitigating metabolic stress responses relevant to ageing and cardiometabolic disease.
Expert Commentary
This well-controlled study adds critical insight into how macronutrient composition within fasting-mimicking diets modulates specific cardiometabolic and molecular outcomes. The selective reduction in visceral adiposity and improvements in autonomic function and microbiome diversity with high-protein FMD suggest protein intake may potentiate therapeutic benefits beyond traditional fasting protocols. These findings align with emerging evidence that variable nutrient sensing and metabolic flux influence autophagic activity and systemic health.
However, the study’s short duration (7 days) and healthy participant population limit generalizability to patients with established metabolic diseases or longer-term clinical endpoints. Further research is needed to elucidate the durability of these effects, potential differential impacts in diverse populations, and mechanistic underpinnings linking protein intake, lipid metabolism, and autophagy.
Conclusion
Both low- and high-protein fasting-mimicking diets promote cardiometabolic health benefits and autophagy induction, yet diverge in specific effects on visceral fat reduction, lipid metabolism, heart rate variability, and gut microbiome diversity. Tailoring FMD macronutrient content can optimize individual outcomes and adherence based on personalized health goals. This study encourages a nuanced approach to dietary fasting therapies for cardiometabolic risk management and healthy ageing.
References
Burns L, Cooper S, Sarmad S, Funke G, Di Mauro A, Gaitanos GC, Tsintzas K. Effects of fasting-mimicking diets with low and high protein content on cardiometabolic health and autophagy: A randomized, parallel group study. Clin Nutr. 2025 Sep;52:299-312. doi: 10.1016/j.clnu.2025.08.004. Epub 2025 Aug 6. PMID: 40816210.