Highlight
Cribriform-positive prostate cancer significantly increases the 15-year risk of metastasis compared to cribriform-negative disease. Radiotherapy combined with neoadjuvant androgen deprivation therapy (ADT) substantially reduces long-term metastasis risk in cribriform-positive patients. Surgery delays metastasis but does not significantly improve long-term outcomes over active monitoring in these cases. Cribriform-negative prostate cancer patients have favorable outcomes with low metastasis incidence across treatment modalities, supporting eligibility for active surveillance.
Study Background
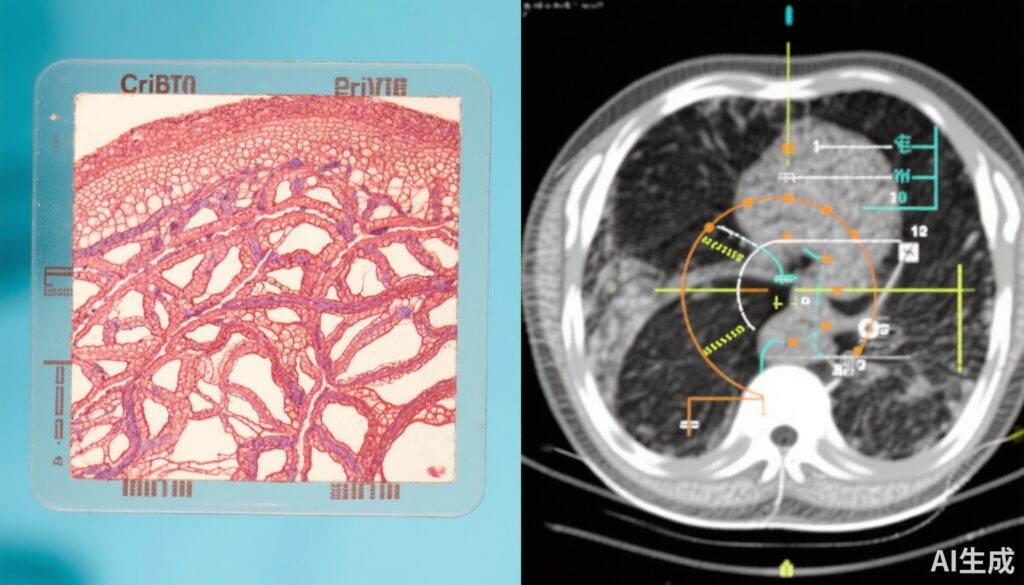
Prostate cancer remains one of the most common malignancies among men worldwide. Histopathologic features, particularly cribriform architecture—comprising invasive cribriform carcinoma and intraductal carcinoma—have been consistently associated with aggressive tumor behavior and poor clinical outcomes. Despite its known prognostic significance, the optimal management strategy for cribriform-positive prostate cancer remains unsettled, especially due to a lack of randomized clinical trial data assessing long-term metastasis risk related to this subtype.
Study Design
The PROTECT trial is a landmark phase 3 randomized clinical trial conducted from 1999 to 2009, enrolling 1,643 men with clinically localized prostate cancer. Participants were randomly assigned to receive one of three management strategies: active monitoring, radical prostatectomy (surgery), or radiotherapy combined with neoadjuvant androgen deprivation therapy (ADT). This secondary analysis retrospectively reviewed biopsy specimens from 712 men available for centralized histopathologic assessment. Patients were classified as cribriform-positive if invasive cribriform carcinoma and/or intraductal carcinoma were identified in the diagnostic biopsy slides. The primary endpoint was progression to metastatic disease, including bony, visceral, or lymph node metastases confirmed on imaging or PSA rising above 100 ng/mL, within 15 years. Both intention-to-treat and per-protocol analyses were conducted, adjusting for key variables such as age, PSA level, Gleason score, and treatment assignment.
Key Findings
Among the 712 men analyzed (mean age 62 years), 93 (13.1%) were cribriform-positive, and 42 (5.9%) developed metastases during follow-up. The presence of cribriform morphology was a potent, independent predictor of metastasis risk. Specifically, cribriform-positive patients had a hazard ratio (HR) of 3.61 (95% CI, 1.60-8.11; P = .003) for metastasis compared to cribriform-negative patients.
Regarding treatment modalities, radiotherapy with neoadjuvant ADT markedly decreased the risk of metastasis in cribriform-positive patients (HR 0.35, 95% CI 0.16-0.78; P = .04), yielding a 15-year cumulative metastasis incidence of approximately 8%. Surgery delayed metastasis relative to active monitoring but did not reach statistical significance for long-term metastasis reduction (HR 0.52, 95% CI 0.25-1.08; P = .09), with 15-year cumulative incidence rates around 26% for surgery and 25% for active monitoring. For patients lacking cribriform morphology, metastasis rates were low across all treatments and demonstrated no significant differences, supporting conservative management strategies like active surveillance.
Per-protocol analyses confirmed these results, reinforcing the notion that cribriform morphology serves as a critical stratifier for metastasis risk and therapeutic response.
Expert Commentary
This secondary analysis of the PROTECT trial provides valuable randomized evidence elucidating how distinct histopathological features influence long-term clinical outcomes in prostate cancer. The strong association of cribriform morphology with metastasis underscores its clinical relevance beyond traditional risk factors such as PSA and Gleason score. The demonstrated effectiveness of radiotherapy with neoadjuvant ADT in substantially reducing metastasis offers a compelling treatment consideration for men harboring cribriform-positive tumors.
However, surgery, while delaying metastasis, did not produce statistically significant long-term benefits versus active monitoring, potentially reflecting limitations in surgical eradication of aggressive tumor clones or residual micrometastatic disease. This finding calls for further investigations exploring combination or multimodal approaches incorporating systemic therapies in this subgroup.
The favorable metastasis profile of cribriform-negative patients supports current trends favoring active surveillance for low-risk prostate cancer, minimizing overtreatment and associated morbidity.
Limitations of this analysis include its retrospective classification of cribriform status and potential selection bias inherent in the subset of patients whose biopsies were available for review. Nonetheless, the rigorous centralized pathology assessment and extended follow-up strengthen its validity.
Conclusion
The PROTECT trial secondary analysis establishes cribriform morphology as a robust independent predictor of long-term metastasis risk in localized prostate cancer. Radiotherapy with neoadjuvant ADT significantly mitigates this risk for cribriform-positive patients, suggesting it should be strongly considered in their treatment planning. Conversely, cribriform-negative patients show excellent outcomes regardless of treatment approach, supporting eligibility for active surveillance protocols. These findings enhance personalized prostate cancer management by integrating histopathologic subtype into risk stratification and therapeutic decision-making.
Funding and Trial Registration
The original PROTECT trial was funded and sponsored as detailed in the primary publications. This secondary analysis was conducted by the study authors with no additional external funding noted. The trial is registered with ClinicalTrials.gov under the identifier NCT02044172.
References
Sushentsev N, Warren AY, Colling R, Verrill C, Pazukhina E, Blyuss O, Seibert TM, Barrett T, Mills IG, Bryant RJ, Donovan JL, Neal DE, Hamdy FC. Active Monitoring, Surgery, and Radiotherapy for Cribriform-Positive and Cribriform-Negative Prostate Cancer: A Secondary Analysis of the PROTECT Randomized Clinical Trial. JAMA Oncol. 2025 Oct 16:e254125. doi: 10.1001/jamaoncol.2025.4125. Epub ahead of print. PMID: 41100113; PMCID: PMC12532030.
Mottet N, van den Bergh RCN, Briers E, et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer. 2023 Edition. Eur Urol. 2023.
Epstein JI, Egevad L, Amin MB, et al. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol. 2016;40(2):244-252.