Study Background and Disease Burden
Metabolic dysfunction-associated steatohepatitis (MASH), also known as non-alcoholic steatohepatitis (NASH), represents a progressive liver disease characterized by hepatic steatosis, inflammation, and varying degrees of fibrosis. It is an increasingly prevalent cause of chronic liver disease worldwide, strongly associated with metabolic comorbidities such as obesity, type 2 diabetes mellitus (T2DM), and insulin resistance. The pathophysiology of MASH implicates dysregulated lipid metabolism, oxidative stress, inflammation, and fibrogenesis. Despite growing disease burden, effective pharmacotherapies remain limited, highlighting an urgent unmet medical need to identify agents that can improve liver histology and prevent progression to cirrhosis and liver-related complications.
Free fatty acid receptors 1 and 4 (FFAR1 and FFAR4), also known as G-protein coupled receptors GPR40 and GPR120 respectively, are expressed on multiple cell types including pancreatic islets and immune cells. They regulate glycaemic control by modulating insulin secretion, and influence inflammatory pathways. This dual role makes them attractive therapeutic targets for MASH, as both glucose metabolism and inflammation contribute to disease progression.
Icosabutate is a novel, orally bioavailable FFAR1/FFAR4 agonist designed to leverage these mechanisms. Preclinical data supported a potential benefit in reducing liver inflammation and fibrosis. The ICONA study was undertaken to evaluate the efficacy and safety of icosabutate in patients with biopsy-confirmed MASH with fibrosis stages F1 to F3, a group at risk for progressive liver disease but generally without advanced cirrhosis.
Study Design
ICONA was a phase IIb, multicentre, 52-week, randomized, double-blind, placebo-controlled trial (NCT04052516). A total of 215 patients with histologically confirmed MASH and fibrosis stages F1 to F3 were enrolled and randomized 1:1:1 to receive once-daily oral icosabutate 300 mg, 600 mg, or placebo for one year.
The primary efficacy endpoint was the proportion of patients in the 600 mg arm achieving resolution of MASH without worsening of fibrosis by histology at week 52. Secondary endpoints included the proportion of patients achieving at least a one-stage improvement in fibrosis, changes in biomarkers of liver injury, inflammation, and glycaemic control. Safety and tolerability were also assessed systematically throughout the study.
Key Findings
The primary efficacy population comprised 187 patients: placebo (n=62), 300 mg icosabutate (n=58), and 600 mg icosabutate (n=67). Baseline demographics and disease characteristics were balanced across groups, with a majority having F2 or F3 fibrosis.
The primary endpoint—MASH resolution without fibrosis worsening—showed a trend favoring the 600 mg icosabutate arm (23.9%) over placebo (14.5%) but did not reach statistical significance (odds ratio [OR] 2.01; 95% confidence interval [CI] 0.8–5.08; p=0.13).
Notably, the secondary endpoint of fibrosis improvement by at least one stage was met more frequently in treated groups. The 300 mg arm showed a statistically significant response rate of 29.3% (OR 2.89, 95% CI 1.09–7.70), and the 600 mg arm a 23.9% response rate (OR 2.4, 95% CI 0.90–6.37), compared to 11.3% in placebo.
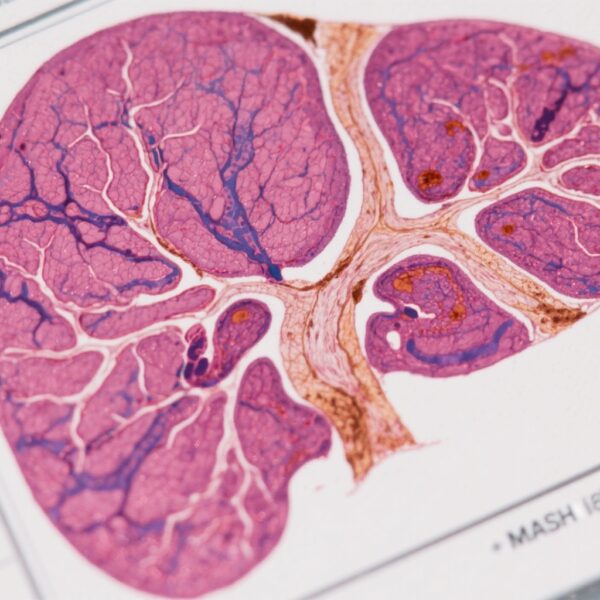
AI-assisted digital pathology analysis corroborated these findings, demonstrating a reduction in fibrotic burden with icosabutate treatment, enhancing objectivity and sensitivity beyond conventional histology.
Non-invasive biomarkers of liver injury (e.g., serum aminotransferases), inflammation (e.g., C-reactive protein), and glycaemic measures improved significantly with icosabutate therapy, supporting the drug’s multifaceted mechanism.
Safety analysis revealed that icosabutate was generally well tolerated. Most treatment-emergent adverse events were mild or moderate, and importantly, there were no reported cases of drug-induced liver injury. This safety profile is encouraging given the chronic treatment nature required for MASH.
Expert Commentary
The ICONA trial’s failure to meet its primary endpoint illustrates the challenges inherent in drug development for MASH, a heterogenous and complex disease. However, the consistent signals of fibrosis improvement and positive biomarker changes suggest biological activity and clinical potential.
The somewhat higher fibrosis response in the 300 mg group compared to 600 mg raises interesting questions about dose response and pharmacodynamics. Further dose-ranging studies may clarify these observations.
Additionally, AI-assisted digital pathology represents a promising advancement in assessing liver histology, providing more granular and quantitative data that may enhance future trial sensitivity and reproducibility.
Given the link between FFAR1/4 signalling and glucose metabolism, subpopulation analyses focusing on patients with concomitant T2DM or more advanced fibrosis (F2-F3) might identify groups with higher treatment responsiveness, aligning with precision medicine approaches.
Study limitations include the relatively small sample size, limited ethnic diversity, and lack of longer-term follow-up data. These factors affect generalizability and assessment of durability of response.
Conclusion
The ICONA phase IIb trial evaluated icosabutate, a dual FFAR1/FFAR4 agonist, in patients with MASH and fibrosis stages F1-F3. Although the primary endpoint of MASH resolution without fibrosis worsening was not met, evidence from histologic fibrosis improvement by conventional and AI methods, coupled with reductions in liver injury and glycaemic biomarkers, supports further clinical development.
Importantly, icosabutate demonstrated a favorable safety and tolerability profile over one year, addressing an essential aspect of long-term therapy for a chronic condition.
Future studies focusing on patients with more advanced fibrosis and metabolic comorbidities, along with exploration of combination regimens, are warranted to delineate the full therapeutic potential of FFAR1/FFAR4 agonism in MASH.
References
Harrison SA, Alkhouri N, Ortiz-Lasanta G, Rudraraju M, Tai D, Wack K, Shah A, Besuyen R, Steineger HH, Fraser DA, Sanyal AJ; ICONA Study Investigators. A phase IIb randomised-controlled trial of the FFAR1/FFAR4 agonist icosabutate in MASH. J Hepatol. 2025 Aug;83(2):293-303. doi: 10.1016/j.jhep.2025.01.032 IF: 33.0 Q1 . Epub 2025 Feb 10. PMID: 39938653 IF: 33.0 Q1 .
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease—Meta‐analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016 Jul;64(1):73-84.
Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006 Dec 14;444(7121):860-7.