Highlight
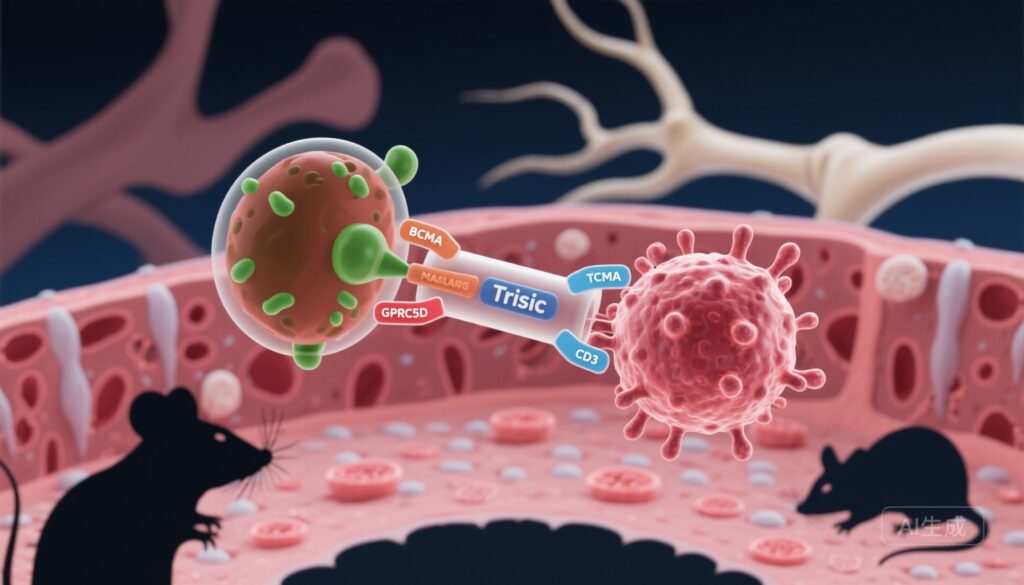
– Ramantamig (JNJ-79635322) is a trispecific T-cell engager directed at BCMA, GPRC5D, and CD3 designed to increase tumor binding avidity and overcome antigen-loss mediated resistance in multiple myeloma (MM).
– In preclinical models, ramantamig produced potent cytotoxicity at sub-nanomolar concentrations, depleted malignant plasma cells in patient ex vivo assays and whole-blood co-cultures, and showed tumor prevention and regression activity in murine xenograft models.
– These data support clinical translation; two phase 1 trials in relapsed/refractory MM (NCT05652335, NCT06768489) are ongoing to evaluate safety, tolerability, pharmacokinetics, and early efficacy.
Background and Unmet Need
Multiple myeloma is a plasma cell malignancy characterized by clonal proliferation within the bone marrow, ongoing genomic evolution, and frequent relapse despite successive lines of therapy. Antigen-directed immunotherapies that recruit endogenous T cells—such as bispecific T-cell engagers and chimeric antigen receptor (CAR) T cells—have transformed outcomes for some patients, particularly those targeting B-cell maturation antigen (BCMA). However, durable control remains challenging because of tumor heterogeneity, antigen downregulation or loss, and the immunosuppressive bone marrow microenvironment.
Dual-targeting approaches aim to mitigate antigen escape and increase target engagement through avidity effects. GPRC5D (G protein–coupled receptor class C group 5 member D) has emerged as a complementary myeloma antigen with high expression on plasma cells and a pattern distinct from BCMA, providing a rationale for simultaneous targeting. Trispecific constructs that co-engage two tumor antigens and CD3 on T cells are designed to increase selectivity for malignant plasma cells, enhance cytotoxic potency, and reduce the opportunity for tumor cells to escape through loss of a single antigen.
Study Design (Preclinical Overview)
The manuscript by Pillarisetti et al. describes the preclinical characterization of ramantamig (JNJ-79635322), a trispecific antibody that binds BCMA and GPRC5D on target cells and CD3 on T cells. The evaluation included in vitro cytotoxicity assays against engineered and multiple myeloma cell lines, assays of T-cell activation, ex vivo co-culture experiments with primary patient bone marrow samples, whole-blood co-culture assays using healthy donor blood with added myeloma cells, and in vivo efficacy studies in immunodeficient murine xenograft models including prevention and regression paradigms.
Key experimental endpoints were tumor-cell killing potency (EC50), T-cell activation markers and cytokine release, depletion of malignant plasma cells in patient-derived samples, and tumor growth inhibition and regression in mouse models. The construct’s activity against cell lines expressing single or both antigens was explicitly tested to probe the added value of dual targeting.
Key Findings
In vitro potency and T‑cell activation
Ramantamig induced potent, concentration-dependent cytotoxicity in multiple myeloma cell lines at sub-nanomolar concentrations, consistent with high functional potency. The trispecific construct activated T cells (upregulation of activation markers and production of effector cytokines) in parallel with tumor-cell lysis. Importantly, ramantamig demonstrated activity against both dual-antigen–expressing and single-antigen–expressing myeloma lines, indicating the construct can mediate cytotoxicity when either BCMA or GPRC5D is present.
Ex vivo depletion of patient malignant plasma cells
In an ex vivo T-cell co-culture assay using bone marrow samples from patients with multiple myeloma, ramantamig produced dose-dependent depletion of malignant plasma cells. The ability to reduce clonal plasma cell populations in primary material is an important translational signal, supporting the construct’s capacity to engage endogenous human T cells and target clinically relevant disease cells.
Whole-blood co-culture—physiologic context
To approximate a more physiological milieu, the authors used fresh whole blood from healthy donors co-cultured with H929 myeloma cells. Under these conditions, ramantamig also elicited dose-dependent tumor-cell depletion, suggesting functional activity in the presence of other blood components and potentially reflecting aspects of target engagement and effector function in the circulation.
In vivo efficacy in xenograft models
Ramantamig showed potent antitumor effects in murine xenograft models. In a prevention model using single-target–expressing clonal cells, ramantamig prevented tumor establishment. In two regression models, the trispecific agent induced tumor shrinkage, supporting both prophylactic- and treatment-context activity in vivo. As with most xenograft studies, these models employ immune-deficient mice reconstituted with human T cells or rely on adoptive transfer to provide effector cells; nonetheless, they provide an important proof-of-concept for in vivo antitumor potency.
Antigen coverage and resistance considerations
The construct’s demonstrated activity against both single and dual antigen-expressing cells is a critical mechanistic observation. Dual targeting increases the chance of recognizing heterogeneous clonal populations within the marrow and reduces selective pressure favoring cells that have downregulated one target antigen. These features could translate into deeper and more durable remissions if confirmed in patients.
Safety Signals and Translational Considerations
The preclinical work focused on efficacy and mechanism; detailed safety and toxicity assessments will require clinical data. Nonetheless, several important translational considerations arise:
- On-target, off-tumor effects: Both BCMA and GPRC5D are enriched on plasma cells, but normal plasma cell depletion is an anticipated on-target effect. GPRC5D expression has also been linked to keratinized tissues (e.g., hair follicles and nails) in some studies; clinical experience with GPRC5D-targeted bispecifics has reported dermatologic and nail abnormalities, which will require monitoring.
- Cytokine release and neurotoxicity: CD3-engaging therapies commonly trigger cytokine release syndrome (CRS) and, less frequently, immune effector cell-associated neurotoxicity syndrome (ICANS). The magnitude and timing of these events depend on dosing, route of administration, and construct-specific properties (affinity and valency) and must be evaluated in early-phase trials.
- T-cell fitness and exhaustion: Sustained antitumor control requires durable T-cell function. Repeated or prolonged T-cell activation can lead to exhaustion; combination strategies or sequential therapies may be needed to preserve or reinvigorate effector function.
- Pharmacokinetics and dosing: Trispecific molecules can have distinct pharmacokinetic (PK) profiles compared with bispecifics or monoclonal antibodies. Optimal dosing regimens to maximize efficacy while limiting toxicity will be determined in phase 1 studies.
Expert Commentary and Limitations
Ramantamig represents a logical extension of the antigen-targeting paradigm in myeloma: by engaging two nonidentical tumor-associated antigens and recruiting T cells, trispecifics aim to improve tumor selectivity and reduce resistance. The preclinical dataset presented shows encouraging potency across multiple complementary assays, including patient-derived material—an important translational step beyond cell-line–only work.
However, important limitations temper enthusiasm pending clinical data. Preclinical xenograft models do not fully recapitulate the human bone marrow microenvironment, immunoregulatory signals, or long-term dynamics of immune-tumor interactions. The safety profile cannot be inferred from efficacy studies; CD3-engaging agents typically require careful dose-escalation and CRS mitigation strategies (e.g., step-up dosing, corticosteroid or IL-6 blockade readiness). Finally, manufacturing complexity and PK behavior of trispecifics can affect scalability and clinical deployment.
Clinical Development and Next Steps
The preclinical dataset has supported the initiation of phase 1 clinical trials in relapsed/refractory multiple myeloma: NCT05652335 and NCT06768489. These studies will define the maximum tolerated dose (MTD) or recommended phase 2 dose (RP2D), characterize safety (with emphasis on CRS, neurotoxicity, and off-tumor effects), assess pharmacokinetics and pharmacodynamics, and provide preliminary efficacy signals including response rates and minimal residual disease (MRD) assessment.
Future clinical questions include how trispecific agents will position relative to existing BCMA-directed modalities (CAR T cells, bispecifics, antibody-drug conjugates), whether they can rescue patients who relapse after BCMA-targeted therapy, and if rational combinations with checkpoint modulation, immune agonists, or microenvironment-targeting agents can enhance durability.
Conclusion
Ramantamig (JNJ-79635322) is a promising trispecific T-cell engager targeting BCMA and GPRC5D with potent preclinical antimyeloma activity across in vitro, ex vivo, and in vivo models. The construct’s ability to target single- and dual-antigen–expressing cells offers a mechanistic advantage for addressing tumor heterogeneity and antigen-loss resistance. Ongoing phase 1 trials will be critical to determine safety, tolerability, and whether the preclinical advantages translate into durable clinical responses for patients with relapsed/refractory multiple myeloma.
Funding and ClinicalTrials.gov
The study was conducted by investigators affiliated with the developing organization and supported by company resources as reported in the source manuscript. Clinical trials registered to evaluate ramantamig in relapsed/refractory myeloma: NCT05652335 and NCT06768489.
References
Pillarisetti K, Yang D, Luistro L, Yao J, Smith M, Vulfson P, Testa J Jr, Ponticiello R, Brodeur SR, Heidrich B, Packman K, Singh S, Attar RM, Elsayed YA, Philippar U. Ramantamig (JNJ-79635322), a novel T-cell-engaging trispecific antibody targeting BCMA, GPRC5D, and CD3, in multiple myeloma models. Blood. 2025 Oct 16:blood.2025030027. doi: 10.1182/blood.2025030027. Epub ahead of print. PMID: 41100731.



This preclinical study demonstrates impressive sub-nanomolar potency of ramantamig, a trispecific T-cell engager simultaneously targeting BCMA and GPRC5D. The dual-antigen approach addresses a critical limitation of single-target immunotherapies: antigen escape. By engaging both BCMA and GPRC5D, ramantamig maintains activity against heterogeneous myeloma cell populations and cells that have downregulated either antigen—a mechanism frequently observed in post-CAR-T or post-bispecific relapses.
Clinical Utility: HIGH (for preclinical data). The construct showed consistent activity across multiple model systems: engineered cell lines, primary patient bone marrow samples, whole-blood co-culture, and xenograft models. The ability to deplete malignant plasma cells in ex vivo patient material is particularly encouraging, as it suggests the mechanism translates to clinically relevant disease biology. The ongoing phase 1 trials (NCT05652335, NCT06768489) will be critical to determine safety and early efficacy signals.
Would I implement this clinically? NOT YET—awaiting phase 1 safety data, but with high interest:
1) Monitor early-phase trial results closely for CRS profile, neurotoxicity incidence, and on-target off-tumor effects (particularly dermatologic toxicity from GPRC5D expression in skin/nails)
2) If safety is acceptable, prioritize enrollment of patients who have relapsed after BCMA-directed therapy (CAR-T, belantamab, teclistamab) to test the antigen-escape hypothesis
3) Evaluate MRD-negative response rates and duration compared with single-target bispecifics as key efficacy benchmarks
4) Consider sequencing strategies: whether trispecifics should be positioned before or after single-target BCMA therapies
5) Prepare institutional infrastructure for step-up dosing protocols and CRS management if approved
Key open question: Does dual targeting truly improve durability, or do other resistance mechanisms (T-cell exhaustion, immunosuppressive microenvironment) dominate in relapsed myeloma? Clinical data will clarify whether the mechanistic advantage translates into prolonged remissions.