Background
Postoperative delirium (POD) is a frequent, serious complication following surgery, notably within the postanaesthesia care unit (PACU). It contributes to increased morbidity, prolonged hospital stay, and significant healthcare costs. Despite advances in perioperative care, accurate early identification and prevention of POD remain challenging. Value-based healthcare emphasizes patient-centered outcomes, leveraging Patient-Reported Outcome Measures (PROMs) and Patient-Reported Experience Measures (PREMs) to inform clinical management. However, their prognostic utility in perioperative settings is underutilized.
This study evaluates whether systematically collected PROMs and PREMs can predict POD, particularly focusing on symptoms such as pain, anxiety, stress, thirst, and nausea, in the context of a perioperative brain care bundle known as the Safe Brain Initiative (SBI). The goal is to enhance risk stratification and personalize interventions to reduce early POD incidence.
Study Design
This prospective observational cohort study was conducted at Salem-Spital Bern, a private hospital within the Hirslanden Hospital Group in Switzerland, from January 2023 to January 2024. The cohort included 1412 adults undergoing elective or urgent surgeries who required PACU admission postoperatively. Patients younger than 18 years, those unable to consent, with language barriers, on postoperative mechanical ventilation, or with signs of preoperative delirium (Nu-DESC > 2) were excluded.
The SBI care bundle, which comprises 18 multidisciplinary, nonpharmacologic strategies targeting perioperative brain health, was implemented. PROMs and PREMs were gathered at four key time points: preoperative preparation (T1), PACU admission (T2), PACU discharge (T3), and the worst recorded symptom during PACU stay (T4). Assessments used Numeric Rating Scales (0–10) for patient-reported pain, anxiety, stress, thirst, nausea, and satisfaction. The primary outcome was POD incidence in the PACU, determined by the Nursing Delirium Screening Scale (Nu-DESC), with scores ≥2 indicating delirium.
Key Findings
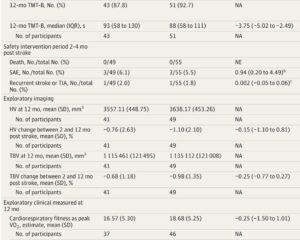
POD occurred in 19.6% (273/1412) of patients. Descriptive analysis showed nearly equal gender distribution, with a mean age of 58.8 years. Surgical duration was significantly associated with POD risk.
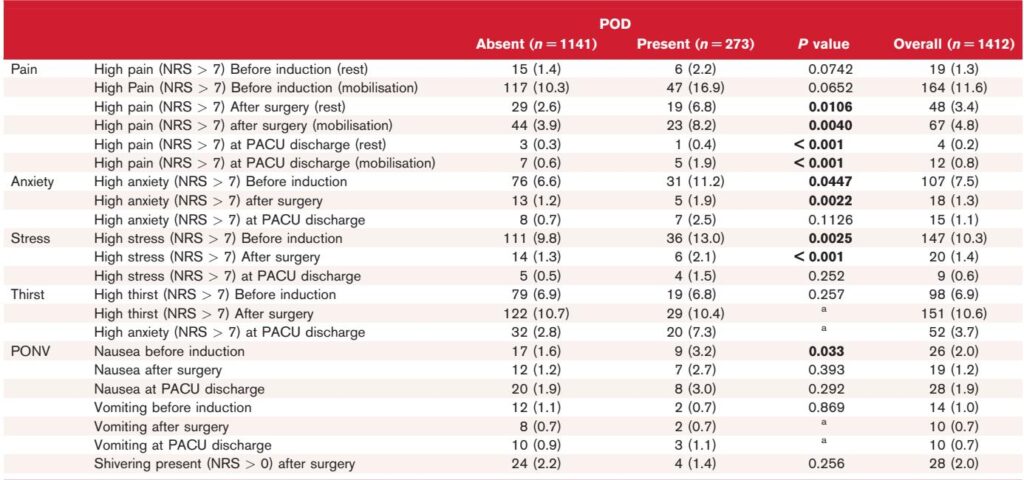
Analysis of PROMs revealed:
– Higher preoperative pain, anxiety, and stress levels in patients who developed POD compared to those who did not.
– Preoperative anxiety (Numeric Rating Scale >7) emerged as an independent predictor of POD with statistical significance (P = 0.012).
– Other factors significantly associated with POD included length of PACU stay, surgical time exceeding 3 hours, type of anesthesia, and elevated preoperative pain during mobilization.
Postoperative symptoms — pain, anxiety, nausea, and vomiting — showed a decreasing trend over time, reflecting improved symptom management likely attributable to the SBI bundle intervention.
Patient-reported experience measures indicated high satisfaction across the cohort, although patients with POD reported consistently lower well-being scores.
Multivariate logistic regression confirmed preoperative anxiety as the strongest independent risk factor for POD. There was potential collinearity among factors such as stress and pain, but anxiety remained the most robust predictor.
Expert Commentary
The study underscores the importance of addressing psychological factors in preoperative assessments. Elevated anxiety may reflect psychological vulnerability or increased stress response, amplifying the risk of delirium in the immediate postoperative period. Importantly, the findings align with recent guidelines discouraging routine benzodiazepine use for anxiety control, advocating instead for nonpharmacological interventions such as enhanced patient education, communication, and engagement to mitigate preoperative anxiety safely.
Implementing the SBI care bundle appears promising in reducing perioperative symptom burden and POD incidence. The systematic integration of PROMs and PREMs facilitates early identification of at-risk patients and informs risk-adjusted care pathways aligning with value-based healthcare.
Limitations include the single-center design, reliance on a single delirium assessment tool (Nu-DESC), and potential confounding due to residual anesthesia effects immediately post-surgery. Additionally, substantial missing data for surgical time required imputation, possibly introducing bias.
Further multicenter research with extended follow-up and comprehensive cognitive assessments is needed to generalize findings and clarify the long-term impact of perioperative brain health bundles.
Conclusion
Preoperative anxiety is a significant independent predictor of postoperative delirium in the PACU, occurring in nearly one-fifth of surgical patients. Patient-reported outcome measures capturing anxiety, pain, and stress provide valuable prognostic information and should be integrated into standard perioperative workflows.
The Safe Brain Initiative care bundle’s implementation has been associated with improved management of postoperative symptoms and a reduction in delirium. These findings advocate for systematic psychological assessments and personalized nonpharmacologic interventions targeting anxiety reduction to optimize perioperative brain health and patient-centered outcomes.
Future studies employing robust statistical methodologies and larger, diverse populations are warranted to validate these results and refine risk stratification models for POD.
References
1. Berger-Estilita J, Marcolino I, Gisselbaek M, et al. Patient-reported outcomes as drivers of postoperative delirium in the postanaesthesia care unit: Data from a one-year prospective cohort study. Eur J Anaesthesiol. 2025 Aug 22. doi: 10.1097/EJA.0000000000002258 IF: 6.8 Q1 . Epub ahead of print. PMID: 40844240 IF: 6.8 Q1 .2. Aldecoa C, Bettelli G, Bilotta F, et al. Update of the European Society of Anaesthesiology and Intensive Care Medicine guideline on postoperative delirium. Eur J Anaesthesiol. 2024;41:81–108.3. Aminpour E, Holzer KJ, Frumkin M, et al. Preoperative predictors of acute postoperative anxiety and depression using ecological momentary assessments. Br J Anaesth. 2024;134:102–110.
4. Meco BC, Jakobsen K, De Robertis E, et al. A first assessment of Safe Brain Initiative care bundle for addressing postoperative delirium. J Clin Anesth. 2024;97:111506.