Highlight
– Imaging-detected extranodal extension (iENE) identifies HPV-positive oropharyngeal cancer patients at increased risk of distant recurrence.
– Grade 3 iENE significantly correlates with worse progression-free survival and higher rates of distant metastasis.
– Incorporation of iENE status into staging systems could improve prognostic accuracy and guide personalized treatment.
– Locoregional control remains comparable regardless of iENE presence, emphasizing distant metastasis as the key adverse outcome.
Study Background
Oropharyngeal cancer (OPC) associated with human papillomavirus (HPV) has a generally favorable prognosis compared to HPV-negative disease, often prompting consideration of treatment deintensification. However, clinical heterogeneity persists, underscoring an unmet need to identify biomarkers that stratify patients by risk. Extranodal extension (ENE) — the spread of cancer beyond the lymph node capsule — is an established pathologic adverse prognostic factor in head and neck cancers. Yet, its assessment typically requires surgical specimens, limiting pre-therapeutic risk stratification in patients managed non-surgically.
Advances in imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) allow visualization of nodal extranodal extension (iENE). Despite its clinical promise, data on the prognostic impact of iENE in HPV-positive OPC remain limited, hindering its incorporation into staging and treatment decisions.
Study Design
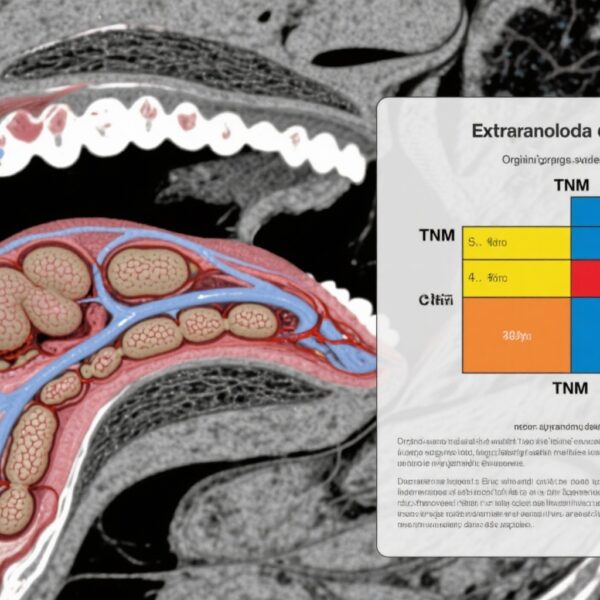
This retrospective cohort study evaluated 421 patients with HPV-positive OPC treated with curative intent between 2009 and 2020 at a tertiary referral hospital. Included patients met criteria of AJCC/UICC TNM 8th edition stages I to III and underwent definitive or postoperative radiation therapy, with or without chemotherapy and/or surgery. Pretreatment CT or MRI scans were reviewed independently by two blinded neuroradiologists to identify and grade iENE based on established semiquantitative criteria: grades 0 (none) through 3 (severe/extensive). Clinical characteristics and outcomes were compared between iENE-positive (iENE+) and iENE-negative (iENE-) groups.
Primary endpoints included progression-free survival (PFS) and rates of distant recurrence. Locoregional control was also assessed. Univariate analyses utilized χ2 and t tests, while multivariate Cox proportional hazards models adjusted for N category, smoking history, chemotherapy regimen, and surgery.
Key Findings
Of the 421 patients, 287 (68%) demonstrated iENE on imaging. Among these, 271 had grade 2 or 3 iENE. The iENE+ cohort had higher nodal burden (mean 4.8 versus 1.9 positive nodes, p < .001) and more frequent involvement of low neck lymph nodes (16% vs 1%, p < .001). Treatment patterns differed, with iENE+ patients more likely to receive chemotherapy (96% vs 79%, p < .001) and less likely to have undergone surgery (7% vs 13%, p = .03).
At 3 years, PFS was significantly lower among iENE+ patients (85%) compared to iENE- patients (94%), corresponding to a hazard ratio (HR) of 2.01 (p = .007). Distant metastasis rates were approximately doubled (16% vs 7%, HR 2.36, p = .031). Locoregional control did not differ significantly (HR 1.35, p = .5).
Analysis by iENE grade revealed that grade 3 iENE conferred the highest risk of adverse outcomes: PFS hazard ratio of 3.56 (p < .001) and distant recurrence HR 3.37 (p = .007). Grade 2 iENE was also associated with increased distant recurrence risk (HR 2.27, p = .041) but not significantly with PFS decline. Lower grades had no statistically significant impact.
Expert Commentary
This study strengthens the evidence that iENE is a clinically meaningful biomarker in HPV-positive OPC, providing noninvasive risk stratification before treatment initiation. The capacity of imaging to detect and grade ENE addresses a critical gap where surgical pathologic evaluation is unavailable or patients are primarily treated nonsurgically.
The pronounced association of high-grade (grade 3) iENE with distant metastasis and PFS failure suggests biologic aggressiveness beyond locoregional spread. Notably, locoregional control did not differ by iENE status, highlighting that iENE primarily portends systemic dissemination risk.
In clinical practice, these findings argue for consideration of iENE assessment when staging HPV-positive OPC, which may refine prognosis and tailor systemic therapy intensity. Incorporation into prospective clinical trials is warranted to validate and possibly recalibrate treatment deintensification strategies in patients without iENE.
Limitations include its retrospective design, potential selection bias, and single-center setting, which may affect generalizability. Validation in external cohorts and prospective designs would strengthen clinical adoption. Additionally, the interobserver discordance in iENE evaluation merits standardized radiologic criteria and training.
Conclusion
Imaging-detected extranodal extension is a significant predictor of increased distant recurrence risk and reduced progression-free survival in patients with HPV-positive oropharyngeal cancer. Grade 3 iENE drives the association with poorer outcomes, while locoregional control remains unaffected by iENE presence. These findings advocate for the integration of iENE into HPV+ OPC staging paradigms to enhance prognostication and optimize therapy selection. Future prospective studies and clinical trials should incorporate iENE status to validate its utility and develop tailored management approaches.
Funding and ClinicalTrials.gov
The original study was conducted at a tertiary referral hospital; funding details were not explicitly provided. No associated clinical trial identifiers were reported.
References
Fan C, Lee J, Stock S, Woody NM, Miller J, Yilmaz E, Scharpf J, Prendes B, Lamarre E, Ku J, Silver N, Geiger JL, Campbell SR, Koyfman SA. Imaging Extranodal Extension (iENE) Predicts Higher Rates of Distant Recurrence for Human Papillomavirus-Positive Oropharyngeal Cancer. Int J Radiat Oncol Biol Phys. 2025 Sep 1;123(1):120-128. doi: 10.1016/j.ijrobp.2025.03.048. Epub 2025 Mar 30. PMID: 40164353.
Additional literature on prognostic imaging biomarkers in HPV-positive OPC and extranodal extension in head and neck cancers supports these findings and underscores their translational relevance.