Highlight
• Low-grade (grade 1) MRI-detected synovitis, tenosynovitis, and osteitis occur frequently in healthy controls and at-risk individuals who do not develop rheumatoid arthritis (RA).
• Such low-grade inflammation is observed at anatomical sites commonly involved in RA, complicating interpretation of MRI findings.
• Inflammation prevalence increases with age across all cohorts.
• Moderate to severe inflammation (grades 2 and 3) are rare in healthy and at-risk non-progressing groups, supporting their higher specificity for RA diagnosis.
Study Background and Disease Burden
Rheumatoid arthritis is a chronic inflammatory autoimmune disease characterized by persistent synovial inflammation leading to joint damage and functional impairment. Magnetic resonance imaging (MRI) is highly sensitive in detecting early joint inflammation, including synovitis, tenosynovitis, and osteitis, often before clinical symptoms become overt. While MRI’s sensitivity is well established, its specificity—ability to distinguish true RA inflammation from other causes—is less well understood. This is critical to minimize false-positive interpretations that may lead to overdiagnosis, unnecessary treatment, and patient distress.
Low-grade inflammation detected by MRI in joints may not always represent RA-specific pathology, as such findings can be present in healthy individuals or those with vague joint pain without progression to RA. This study aims to clarify the frequency and distribution of MRI-detected inflammation in healthy controls and two at-risk cohorts—patients with clinically suspect arthralgia (CSA) and undifferentiated arthritis (UA) who did not progress to RA—compared to patients with established RA. Understanding these patterns could enhance MRI interpretative accuracy and clinical decision-making.
Study Design
This is a longitudinal cohort study combining data from two prospective observational cohorts at Leiden University Medical Centre, Netherlands: the Leiden Early Arthritis Clinic (EAC) and the clinically suspect arthralgia (CSA) cohort, supplemented by a healthy volunteer control group from the same institution.
Participants included:
- 516 patients with RA (diagnosed at or after baseline),
- 305 patients with UA not progressing to RA during one-year follow-up,
- 598 individuals with CSA not progressing to RA during two-year follow-up, and
- 193 healthy volunteers without inflammatory joint disease.
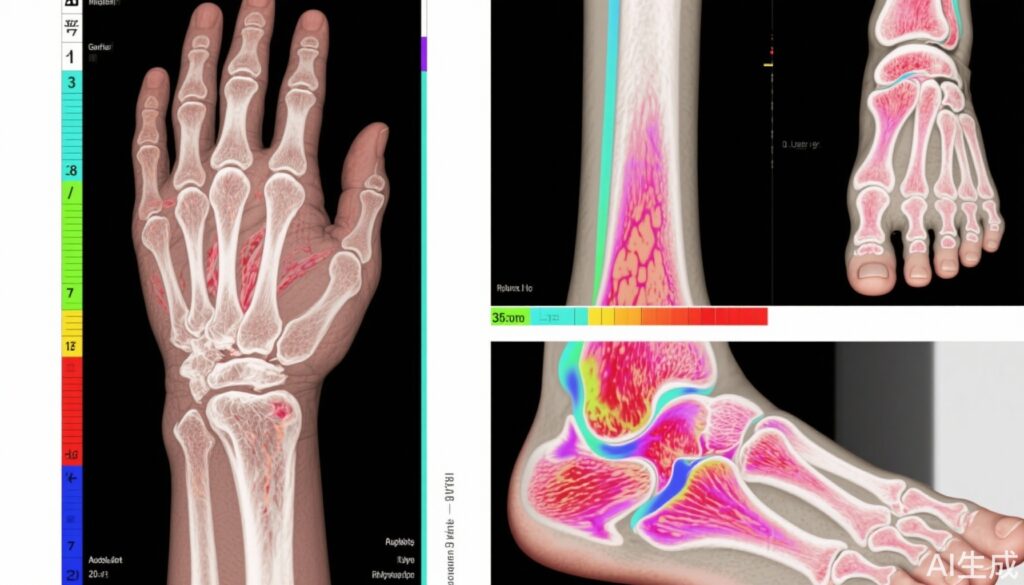
MRI scans were obtained of second to fifth metacarpophalangeal (MCP) joints, wrists, and first to fifth metatarsophalangeal (MTP) joints. Images were contrast-enhanced and assessed for synovitis, tenosynovitis, osteitis, and intermetatarsal bursitis using the Rheumatoid Arthritis MRI Scoring (RAMRIS) system. Two independent blinded readers scored inflammation at each site on a scale from 0 (no inflammation) to 3 (severe inflammation).
Inflammation with a similar grade seen in more than 5% of any reference population (healthy controls or non-progressing at-risk groups) was considered less RA-specific. Data were stratified by age groups: under 40 years, 40-59 years, and 60 years or older. Patient involvement was integrated in cohort design.
Key Findings
The study included 1612 participants, predominantly female (68%) and White (94%), with a mean age of 51 years (SD 14). Key results include:
- Grade 2 and 3 Inflammation: Moderate to severe synovitis, tenosynovitis, or osteitis (grades 2 or 3) were uncommon in healthy controls and CSA non-converters across all ages (occurring in less than 5% of individuals), indicating high specificity for RA.
- Grade 1 Inflammation Prevalence: Low-grade (grade 1) inflammation was prevalent at multiple joint sites in healthy controls and at-risk groups (both CSA and UA non-progressors), exceeding 5% occurrence across all age groups. Notably, these locations overlapped with areas frequently inflamed in RA patients.
- Age-Related Increase: Frequency of low-grade inflammation increased with age in all cohorts, highlighting age as a confounder in MRI interpretation.
- Moderate Inflammation in Older Non-Progressors: Grade 2 inflammation above 5% prevalence was found only in non-progressing UA patients aged 60 or above, suggesting some moderate MRI findings may not always predict RA progression.
The implication is that certain low-grade MRI signals—previously presumed indicative of early RA—can occur in non-inflammatory or non-RA populations, emphasizing caution to avoid overdiagnosis based on mild MRI changes alone.
Expert Commentary
This pioneering study addresses an important gap by evaluating the specificity of MRI findings in inflammatory arthritis and the risk of false positives. Clinical interpretation of MRI must integrate recognition that low-grade inflammation may frequently occur in healthy or at-risk but non-progressing individuals. The standard RAMRIS scoring system remains a valuable tool, but clinical context and degree of inflammation (focusing on moderate to severe grades) should guide diagnostic decisions.
Age stratification reveals that degenerative or subclinical inflammatory changes increase with aging, necessitating age-adjusted MRI thresholds or interpretation guidelines. The unexpected finding of moderate inflammation in non-progressing elderly UA patients warrants further research into benign inflammatory processes mimicking RA on MRI.
Limitations include a predominantly White cohort limiting generalizability to other ethnicities, and follow-up durations that might miss late RA conversion. Additionally, MRI acquisitions were performed within a single center, which may influence reproducibility across varying clinical settings.
Conclusion
This study highlights that low-grade MRI-detected synovitis, tenosynovitis, and osteitis at typical RA sites occur frequently in healthy controls and at-risk individuals who do not develop RA, particularly increasing with age. Moderate to severe MRI inflammation remains more specific to RA. These findings advocate caution against overinterpretation of mild MRI inflammatory signs to reduce false-positive diagnoses and overtreatment.
In clinical practice, combining MRI findings with clinical, serological, and demographic data remains essential to improve diagnostic precision. Future research should aim at refining MRI scoring thresholds incorporating age and investigating mechanisms underlying MRI inflammation in non-RA populations.
References
- Ton DA, den Hollander NK, van Steenbergen HW, van der Helm-van Mil AHM. Comparison of findings on contrast-enhanced MRI of the hand, wrist, and forefoot in healthy controls, two at-risk groups, and patients with rheumatoid arthritis: a cohort study. Lancet Rheumatol. 2025 Sep;7(9):e618-e628. doi: 10.1016/S2665-9913(25)00065-7. PMID: 40523380.
- Van der Heijde D, et al. Magnetic resonance imaging in early arthritis. Nat Rev Rheumatol. 2015 Apr;11(4):279-90. doi: 10.1038/nrrheum.2015.4.
- Østergaard M, et al. Imaging in early rheumatoid arthritis: possibilities and limitations. Nat Rev Rheumatol. 2018 Dec;14(12):669-676. doi: 10.1038/s41584-018-0104-4.